Understanding Bipolar Disorder – Beyond Mood Swings
“They were fine last week—why are they suddenly like this?”
One of the hardest parts for families to grasp is that bipolar disorder isn’t just moodiness. It’s a complex neurobiological condition with episodic highs and lows, often separated by periods of apparent normalcy.
In this post, we break down the basics of bipolar disorder—not from a textbook, but in a way that helps you understand what’s really happening inside the brain, so you can support more effectively.
🧠 What Is Bipolar Disorder?
Bipolar disorder is a mood disorder characterized by alternating episodes of:
-
Mania or Hypomania (high energy, impulsivity, grandiosity)
-
Depression (low energy, hopelessness, withdrawal)
These shifts are not under voluntary control. They are driven by neurochemical and circadian disruptions, not personality flaws or attitude.
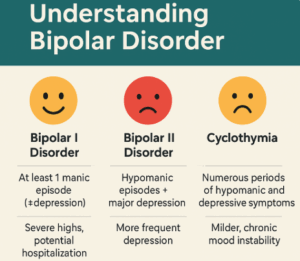
🔍 Types of Bipolar Disorder (Simplified)
| Type | Key Features | Common Presentation |
|---|---|---|
| Bipolar I | At least 1 full manic episode (+/- depression) | May require hospitalization during mania |
| Bipolar II | Hypomania + major depression | Often missed as just “depression” |
| Cyclothymia | Mild highs and lows over 2+ years | Mood instability, but not full episodes |
| Mixed States | Symptoms of mania and depression at the same time | Irritable, anxious, confused presentations |
🕰️ What a Cycle Might Look Like
Let’s take a simplified example:
January: Overworking, barely sleeping, feels “on top of the world” → hypomania
February: Irritable, picking fights, impulsive spending → escalating into mania
March: Crashes into guilt, shame, suicidal thoughts → depressive phase
April: Stabilizes, seems “normal” → inter-episode recovery
June: Relapse begins again due to disrupted sleep or medication drop
Each person’s pattern varies, but families must learn to map this pattern, not just react to the behavior.
🧠 What’s Happening in the Brain?
-
Dysregulation in dopamine and serotonin systems
-
Altered circadian rhythm (sleep–wake cycle)
-
Abnormal activity in prefrontal cortex (judgment) and limbic system (emotion)
🧠 Key takeaway: Bipolar is a brain-based rhythm disorder, not a character issue.
⚠️ Common Myths Families Hold
-
“They’re just being dramatic.”
→ Mania isn’t attention-seeking. It’s a clinical emergency. -
“They were better. Why did they stop medication?”
→ Insight can be impaired in bipolar, especially during highs. -
“They were laughing yesterday. They can’t be depressed today.”
→ Mixed states can cause mood overlap and rapid shifts.
🧭 What Families Can Do
-
Learn to recognize early signs of episodes (we’ll cover this in Post 3)
-
Stop taking every outburst personally—it’s not about you
-
Speak in terms of patterns, not moral judgments (e.g., “This looks like your manic phase” vs. “You’re being irresponsible again”)
💬 Takeaway
When families shift from confusion to comprehension, they become partners in recovery.
In the next post, we’ll explore how to detect early warning signs of both mania and depression—so you can act before things escalate.
👨⚕️ About the Author
Dr. Srinivas Rajkumar T, MBBS, MD (Psychiatry)
Consultant Psychiatrist | Apollo Clinics Velachery & Tambaram
Educator, Family Therapist, and Mood Disorder Specialist
🌐 More content: www.srinivasaiims.com
📞 Appointments: 85951 55808
📩 Connect: Dr. Srinivas Rajkumar T – LinkedIn