Autism and Sleep Problems: Why It Happens and What You Can Do
 😴 Why Sleep Is a Struggle in Autism
😴 Why Sleep Is a Struggle in Autism
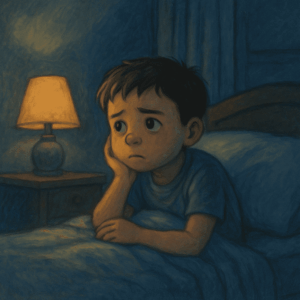
Sleep disturbances affect 40–80% of children with autism. Parents often say:
“He’s awake till 2 AM.”
“She sleeps in short bursts and wakes often.”
“We’re all exhausted.”
Sleep is critical for brain development, emotional regulation, and learning—so addressing it improves both child and family well-being.
🧠 What Causes Sleep Issues in Autism?
-
Melatonin Dysregulation: The hormone that controls sleep-wake cycles may be produced irregularly.
-
Sensory Sensitivities: Even small sounds, textures, or changes in light can disturb sleep.
-
Anxiety and Rigidity: Autistic children may struggle with transitions, including going to bed.
-
Poor Body Awareness: Difficulty recognizing tiredness or internal cues.
-
Co-occurring Conditions: Like ADHD, epilepsy, or gastrointestinal discomfort.
🔍 Common Sleep Problems in Autism
| Type of Problem | Examples |
|---|---|
| Difficulty Falling Asleep | Takes >1 hour to fall asleep, restless |
| Night Wakings | Frequent awakenings, difficulty returning to sleep |
| Early Morning Waking | Wakes at 4–5 AM, won’t go back to sleep |
| Irregular Sleep-Wake Patterns | Sleeps during day, awake at night |
| Resistance to Sleep | Tantrums, hyperactivity before bedtime |
🛠️ Evidence-Based Sleep Strategies
1. Sleep Hygiene Routine
-
Fixed bedtime and wake time—even on weekends
-
Dim lighting 1 hour before sleep
-
Avoid screen time 1–2 hours before bed
-
Calming activities like reading or white noise
2. Sensory Adaptations
-
Weighted blankets for calming proprioceptive input
-
Blackout curtains, white noise machines
-
Comfortable sleepwear and temperature control
3. Visual Schedules and Social Stories
Use bedtime charts or storybooks that outline the steps to bedtime:
-
Brush teeth
-
Change clothes
-
Read book
-
Lights off
Make the routine predictable and easy to follow.
4. Melatonin Supplementation
In select cases, under medical supervision, melatonin (0.5–3 mg) can help initiate sleep. Not a cure, but useful when other methods fail.
⚠️ Always consult a psychiatrist or pediatrician before giving supplements.
5. Daytime Regulation
-
Plenty of physical activity
-
Exposure to natural sunlight in the morning
-
Balanced meals, not heavy dinners
💬 Real-Life Example
Nikhil, age 6, would fall asleep only at midnight and wake frequently. With a visual sleep chart, a consistent winding-down routine, and a mild dose of melatonin, he now sleeps by 9:30 PM and wakes refreshed. His tantrums and hyperactivity have reduced significantly.
📌 When to Seek Help
-
Child is sleep-deprived and irritable
-
Family sleep is severely disrupted
-
Non-pharmacological strategies have failed
-
Suspected coexisting disorders (like epilepsy or reflux)
📍 Dr. Srinivas Rajkumar T
Consultant Psychiatrist – Child, Adolescent & Geriatric Psychiatry
Apollo Clinics Velachery & Tambaram | Mind & Memory Lab
🌐 www.srinivasaiims.com | 📞 +91 85951 55808
Offering holistic autism care including sleep management, sensory integration, and behavior therapy.