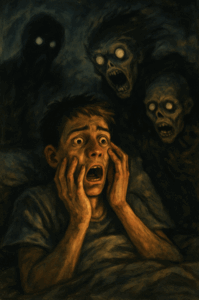
Medicines for Nightmares – What Helps and What to Avoid
 When nightmares become persistent and distressing, non-drug therapies like Image Rehearsal Therapy (IRT) or CBT are usually the first line of treatment. But what if therapy alone isn’t enough? Or what if the nightmares are severe, trauma-related, and deeply embedded?
When nightmares become persistent and distressing, non-drug therapies like Image Rehearsal Therapy (IRT) or CBT are usually the first line of treatment. But what if therapy alone isn’t enough? Or what if the nightmares are severe, trauma-related, and deeply embedded?
In such cases, medications may be considered. But unlike other psychiatric symptoms, nightmares don’t respond well to all drugs — and some may even make things worse.
Let’s explore the evidence behind medications used in nightmare disorder, based on the American Academy of Sleep Medicine (AASM) position paper.
When Are Medications Used?
-
When therapy is not accessible, not effective, or declined by the patient
-
In cases of severe PTSD-associated nightmares
-
When nightmares occur alongside other psychiatric conditions
-
When patients prefer a combined approach (therapy + medication)
Medications That May Be Used
(These have supportive evidence, though not all are first-line.)
1. Prazosin
💊 An alpha-1 adrenergic blocker that reduces norepinephrine-driven hyperarousal
✅ Most studied drug for PTSD-related nightmares
📊 Studies show >50% reduction in nightmare frequency and distress
⚠️ Side effects: dizziness, hypotension; careful dose titration needed
2. Triazolam & Nitrazepam
💤 Short-acting benzodiazepines occasionally used in idiopathic nightmares
📉 Reduce REM sleep, but risk dependency
⚠️ Use with caution and only short term
3. Antidepressants & Others (used in PTSD-related nightmares)
-
Trazodone
-
Fluvoxamine
-
Cyproheptadine
-
Phenelzine (MAOI)
-
Gabapentin
-
Topiramate
-
Tricyclic antidepressants (e.g., amitriptyline)
-
Nabilone (cannabinoid derivative)
-
Clonidine
-
Atypical antipsychotics (Olanzapine, Risperidone, Aripiprazole)
⚠️ Many of these are not specifically approved for nightmares, but have shown benefit in PTSD populations. Always consider comorbidities, side effects, and polypharmacy risks.
Medications Not Recommended
According to AASM, these are not effective and may worsen nightmares:
-
Clonazepam: Often worsens sleep architecture and can lead to rebound nightmares
-
Venlafaxine: Associated with increased dream intensity and nightmares, especially at higher doses
Important Considerations
-
Nightmares are not always pharmacological problems
-
Avoid using medication as a first choice unless absolutely necessary
-
Discontinue medications causing REM rebound gradually (e.g., certain antidepressants, benzodiazepines)
-
Tailor the treatment to each individual: their symptoms, psychiatric profile, and goals
Coming Up Next
In the next article, we’ll explore how to track and measure nightmares using reliable tools like the CAPS scale, PSQI, and sleep diaries.
About the Author
Dr. Srinivas Rajkumar T
Consultant Psychiatrist
Apollo Clinics – Velachery & Tambaram, Chennai
📞 Phone: 8595155808
🌐 www.srinivasaiims.com
💊 Advocating for cautious, personalized use of medication in sleep and trauma-related conditions
Medications may offer short-term relief, but the real power lies in understanding the root of the nightmare. A comprehensive plan — not just a pill — is what truly heals.