One Size Doesn’t Fit All – Personalizing Treatment for Nightmare Disorder
 By now, we’ve explored the many ways nightmare disorder can be treated — from Image Rehearsal Therapy to prazosin, from sleep hygiene to lucid dreaming. But here’s the real challenge: not every person with nightmares responds to the same approach.
By now, we’ve explored the many ways nightmare disorder can be treated — from Image Rehearsal Therapy to prazosin, from sleep hygiene to lucid dreaming. But here’s the real challenge: not every person with nightmares responds to the same approach.
That’s why the final step in managing nightmare disorder is learning to personalize the treatment plan — matching the intervention to the person, not just the diagnosis.
Key Factors to Consider Before Choosing a Treatment
✅ 1. Is the nightmare trauma-related?
-
If yes: Consider IRT, ERRT, EMDR, or prazosin
-
If no/idiopathic: General CBT, lucid dreaming, hypnosis, or relaxation techniques may help
✅ 2. Are there coexisting conditions?
-
PTSD, depression, anxiety, borderline personality: Go for structured therapies like IRT + medication
-
Insomnia: Add CBT-I to the plan
-
Substance use or REM-rebound: Address the underlying cause first
✅ 3. How distressing are the nightmares?
-
Mild to moderate → Behavioral strategies often suffice
-
Severe, frequent, or sleep-disrupting → May need pharmacological support in the short term
✅ 4. What does the patient prefer?
-
Some prefer non-drug approaches
-
Others may be too distressed or cognitively burdened for therapy and want symptom relief first
-
Clinician and patient should decide together based on shared goals
Recommended → May Be Used → Not Recommended
The AASM Position Paper organizes treatment strategies into three tiers:
| Category | Examples |
|---|---|
| Recommended | Image Rehearsal Therapy (IRT) |
| May be used | CBT, CBT-I, EMDR, ERRT, prazosin, fluvoxamine, gabapentin, lucid dreaming, hypnosis, topiramate, trazodone, progressive relaxation, etc. |
| Not recommended | Clonazepam, venlafaxine |
This doesn’t mean “not recommended” drugs are dangerous in all cases — just that risks outweigh benefits for most people.
The Clinician’s Role in Personalized Care
As psychiatrists and mental health professionals, our role is to:
-
Understand the patient’s nightmare profile
-
Evaluate psychiatric comorbidities
-
Respect patient autonomy and insight
-
Start small – often behavioral therapies are low-risk, high-benefit
-
Adjust based on feedback and tracking (using CAPS, PSQI, or dream logs)
No treatment plan is static. What works today may need a tweak tomorrow.
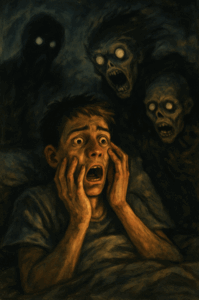
Patient Story: “From Fear to Freedom”
Ravi, a 32-year-old software engineer, struggled with vivid nightmares after surviving a major accident. He avoided sleep, became irritable, and started drinking to cope. Instead of jumping to medication, his psychiatrist helped him:
-
Begin Image Rehearsal Therapy
-
Practice relaxation breathing before bed
-
Taper off alcohol with support
-
Later add low-dose prazosin for breakthrough nightmares
Three months later, he’s sleeping better — and dreaming of life again.
Coming Up Next
In the final article of this series, we’ll offer a full summary and checklist for clinicians and patients — including what to ask, what to track, and how to follow up.
About the Author
Dr. Srinivas Rajkumar T
Consultant Psychiatrist
Apollo Clinics – Velachery & Tambaram, Chennai
📞 Phone: 8595155808
🌐 www.srinivasaiims.com
🧩 Personalized psychiatry that respects your story and science
In sleep medicine, as in life, there’s no magic bullet. But with the right mix of tools, trust, and timing — even the most stubborn nightmares can lose their power.