Anorexia Nervosa: When the Mirror Lies
 Introduction
Introduction
Anorexia Nervosa is not just a refusal to eat or a desire to be thin—it’s a serious psychiatric disorder where distorted body image and intense fear of weight gain override the body’s natural hunger signals. It affects both the mind and the body and, if left untreated, can be life-threatening.
What is Anorexia Nervosa?
Anorexia Nervosa is an eating disorder characterized by:
-
Restrictive eating leading to significantly low body weight
-
Intense fear of gaining weight or becoming fat, even if underweight
-
Distorted perception of body size or shape
It is classified as a mental illness in the ICD-11 and DSM-5, often overlapping with depression, anxiety disorders, and obsessive-compulsive traits.
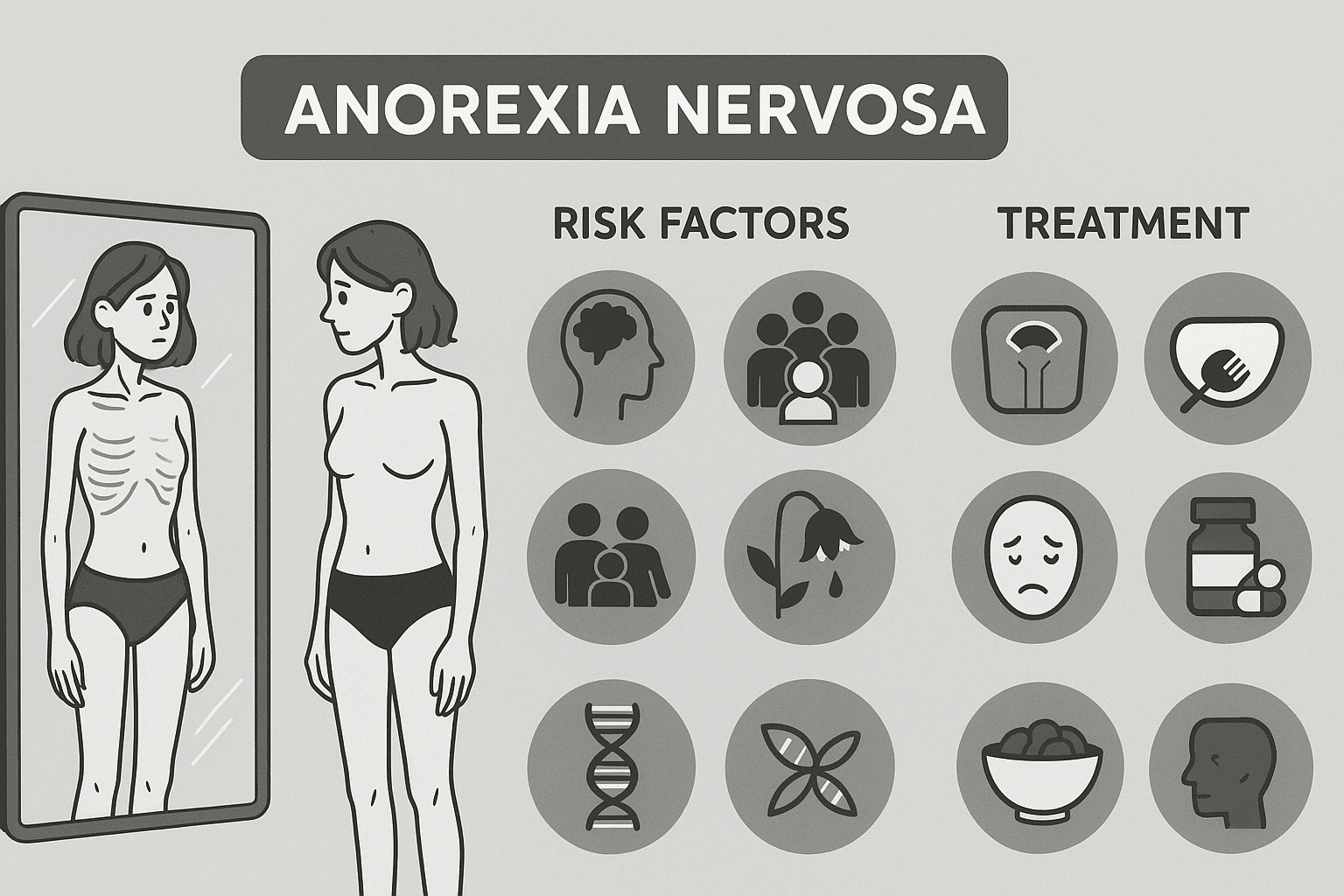
Who is at Risk?
While anorexia most commonly begins in adolescence, it can affect people of any age, gender, or background.
Common risk factors include:
-
Psychological traits: Perfectionism, low self-esteem, high need for control
-
Social pressure: Beauty standards glorifying thinness, especially on social media
-
Family dynamics: Enmeshed families or high parental expectations
-
Biological factors: Genetic predisposition, neurotransmitter imbalances (e.g., serotonin, dopamine)
Warning Signs and Symptoms
Physical:
-
Rapid weight loss or being underweight
-
Fatigue, dizziness, and fainting
-
Loss of menstrual periods (amenorrhea)
-
Cold intolerance, dry skin, hair loss
Behavioral and Psychological:
-
Calorie counting, skipping meals, or eating in secret
-
Compulsive exercise
-
Denial of hunger or refusal to eat
-
Preoccupation with food, body shape, or weight
-
Irritability, depression, or emotional withdrawal
Diagnosis
Diagnosis is clinical, based on DSM-5/ICD-11 criteria. Medical investigations rule out physical causes and assess complications.
Key components of assessment:
-
BMI below 17.5 or significant weight loss
-
Body image distortion
-
Endocrine abnormalities (e.g., low estrogen/testosterone)
-
Blood tests may show anemia, electrolyte imbalance, low glucose, or liver enzyme changes
Complications
Anorexia affects almost every system in the body:
-
Cardiac: Bradycardia, hypotension, arrhythmias
-
Reproductive: Infertility, amenorrhea
-
Skeletal: Osteoporosis, fractures
-
Neurocognitive: Poor concentration, memory issues
-
Renal and GI: Constipation, dehydration, electrolyte imbalance
Severe cases may lead to organ failure or sudden cardiac death.
Treatment Approach
Treatment is multidisciplinary, involving:
1. Nutritional Rehabilitation
-
Supervised refeeding plans to restore weight
-
Monitoring for refeeding syndrome in severely malnourished patients
2. Psychotherapy
-
Cognitive Behavioral Therapy (CBT-E): Corrects distorted thinking and helps with weight normalization
-
Family-Based Therapy (FBT): Especially effective for adolescents
-
Psychodynamic therapy: Explores underlying emotional conflicts
3. Medication
-
SSRIs (like fluoxetine) for co-morbid depression or OCD
-
Atypical antipsychotics (like olanzapine) may be used to reduce anxiety and obsessional thinking around food
-
No medication is FDA-approved solely for anorexia itself
4. Hospitalization
-
Required for:
-
BMI < 15
-
Severe electrolyte imbalances
-
Suicidal thoughts
-
Cardiac instability
-
Prognosis
Recovery is possible, but it may be long-term and non-linear. About:
-
50% recover fully
-
30% show partial improvement
-
20% remain chronically ill
Early intervention significantly improves outcomes.
What Can Families Do?
-
Avoid blaming the individual
-
Provide emotional support without pressuring about food
-
Seek professional help early
-
Learn about boundaries and relapse prevention
Conclusion: Seeing Beyond the Mirror
Anorexia Nervosa is not a lifestyle choice. It’s a complex psychiatric condition needing compassionate care, structured support, and a scientific approach. In our image-driven world, it’s essential to promote body neutrality, mental well-being, and early screening in schools and colleges.
If you or someone you know is struggling with disordered eating, reach out. Healing begins when silence ends.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS)
Consultant Psychiatrist
Apollo Clinic, Opp. Phoenix Marketcity, Velachery, Chennai
📞 85951 55808
🌐 srinivasaiims.com