mECT: Precision, Progress, and Proven Power
 Introduction: A Therapy Misunderstood
Introduction: A Therapy Misunderstood
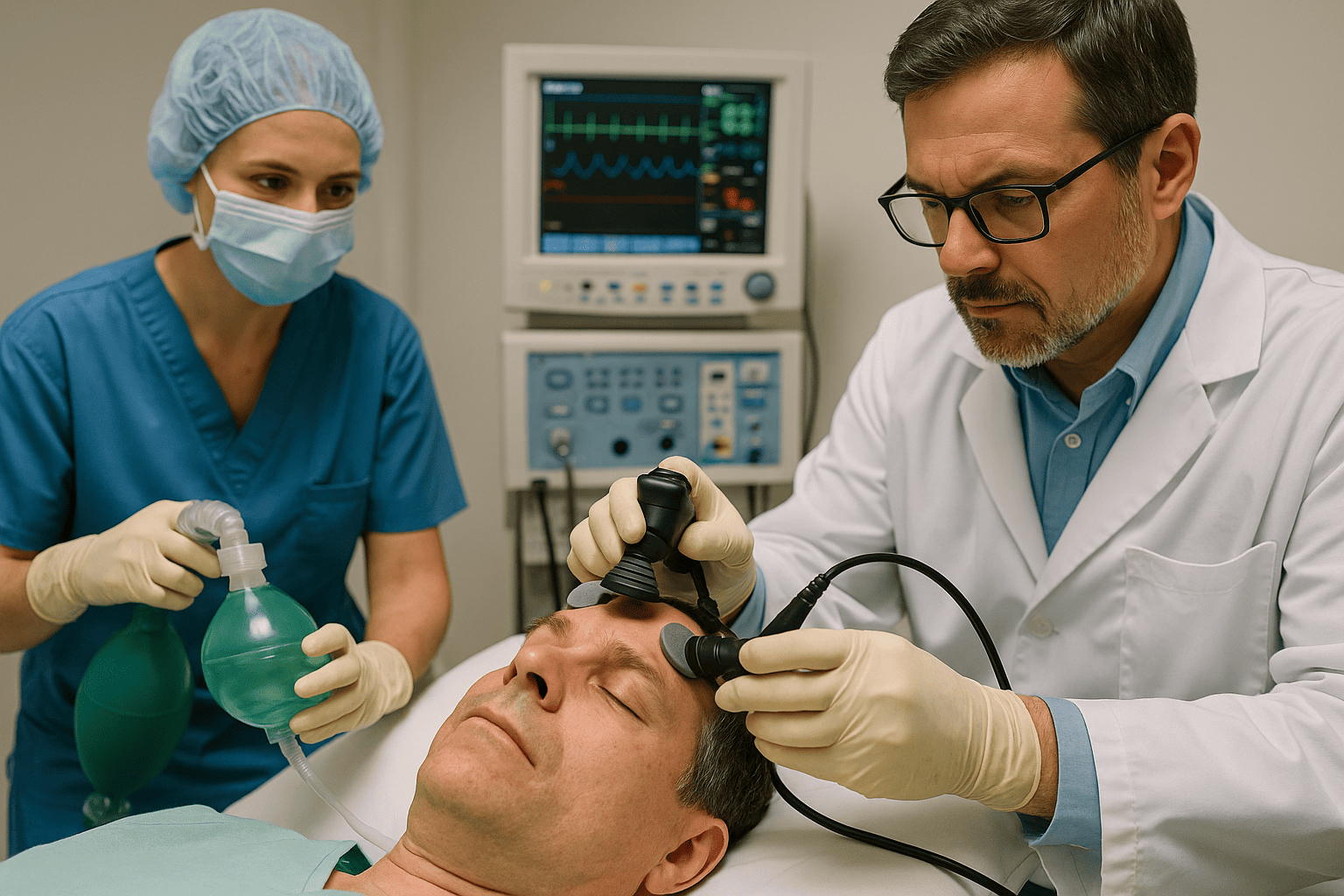
Modern Electroconvulsive Therapy (mECT) often carries the burden of its own history—shrouded in stigma, sensationalism, and outdated imagery. But today’s ECT is nothing like its cinematic caricature. It is anesthetized, titrated, targeted, and above all—scientific.
With decades of refinement, mECT has evolved into one of the safest, most effective treatments in psychiatry, especially in life-threatening conditions like suicidal depression, catatonia, and psychotic disorders. It is time we replace fear with facts.
From Shock to Precision
Modern mECT is performed in a controlled hospital setting with:
-
Short-acting anesthesia
-
Muscle relaxants to prevent injury
-
Cardiac and neurological monitoring
-
Personalized seizure threshold titration
This ensures the patient experiences no pain, while the treatment delivers its therapeutic benefit with maximum safety.
Scientific Advancements in mECT
🔹 1. Titration-Based Dosing
Rather than applying a fixed dose, current protocols estimate an individual’s seizure threshold in the first session and adjust the stimulus accordingly.
Why it matters:
-
Reduces unnecessary electrical exposure
-
Minimizes side effects
-
Optimizes therapeutic response
🔹 2. Ultra-Brief Pulse ECT (UBP-ECT)
Traditional ECT used longer pulses (1.0–1.5 ms). Today, ultra-brief pulses (0.25–0.3 ms) are used to stimulate brain regions more precisely, while sparing surrounding areas.
Benefits:
-
Dramatically reduced cognitive side effects
-
Equally effective in many patients
-
Preferred for elderly or medically fragile patients
🔹 3. Modern Electrode Placement
No more one-size-fits-all. The electrode placement now depends on the clinical context:
| Placement | Use | Advantage |
|---|---|---|
| Right Unilateral (RUL) | Depression | Cognition-sparing |
| Bitemporal | Catatonia, Psychosis | Faster response |
| Bifrontal | Bipolar, Psychotic Depression | Balance between speed & safety |
What Makes mECT Unique?
-
Fastest antidepressant effect—often within days
-
Only first-line treatment for catatonia
-
Effective even when multiple medications have failed
-
Can be used safely during pregnancy
-
Reduces hospital stay and suicide risk
Is It Safe?
Yes. Modern ECT is statistically safer than childbirth.
Side effects may include:
-
Temporary headache or confusion
-
Mild memory disturbances (mostly short-term)
-
Very rare complications with proper pre-anesthetic assessment
In India, MHCA 2017 ensures that ECT is only administered:
-
With informed consent
-
In licensed mental health establishments
-
Under modified (anesthetized) conditions
Addressing the Common Misperceptions
| Myth | Truth |
|---|---|
| “ECT is painful” | Modern ECT is done under full anesthesia |
| “It causes permanent memory loss” | Short-term memory issues may occur but are often reversible |
| “Only used as a last resort” | ECT is often a first-line option in specific situations |
| “It’s outdated” | Modern mECT uses advanced technology and monitoring |
In My Clinical Practice
As a psychiatrist, I have seen mECT transform patients who were mute, immobile, or suicidal. Often within a few sessions, families are amazed to see their loved ones begin eating, speaking, or smiling again—something medications alone hadn’t achieved in months.
Conclusion: A Therapy Refined by Time and Technology
mECT is not a relic of the past—it is psychiatry’s unsung hero.
With its blend of precision, progress, and proven power, it continues to save lives, restore function, and offer hope where none seemed possible.
Let us not allow outdated myths to stand in the way of scientific healing.
Need Help or Second Opinion?
Dr. Srinivas Rajkumar T, MD (AIIMS)
Consultant Psychiatrist
📍 Apollo Clinic, Opp. Phoenix Marketcity, Velachery, Chennai
📞 8595155808
🌐 www.srinivasaiims.com
Specialist in advanced treatments: mECT, tDCS, rTMS, and comprehensive mental health care.