Neurofeedback for ADHD
 Commonly Used Protocols, Evidence, and the Myndlift-Based Model
Commonly Used Protocols, Evidence, and the Myndlift-Based Model
ADHD is one of the few psychiatric conditions where the core deficit—attention regulation—is directly trainable. This makes neurofeedback not an alternative curiosity, but a logically aligned intervention.
Yet neurofeedback for ADHD is also one of the most misunderstood areas in psychiatry. Critics dismiss it as placebo-driven; enthusiasts oversell it as a cure. The truth, as usual, lies in disciplined application, protocol selection, and outcome monitoring.
This article outlines commonly used neurofeedback protocols in ADHD, the current evidence base, and how Myndlift fits into modern, clinician-guided practice.
Why Neurofeedback Makes Sense in ADHD
ADHD is not defined by a lesion or a single biomarker. It is a disorder of self-regulation, involving distributed attentional and executive networks. Traditional treatment addresses this indirectly—through medication, behavioral scaffolding, and environmental modification.
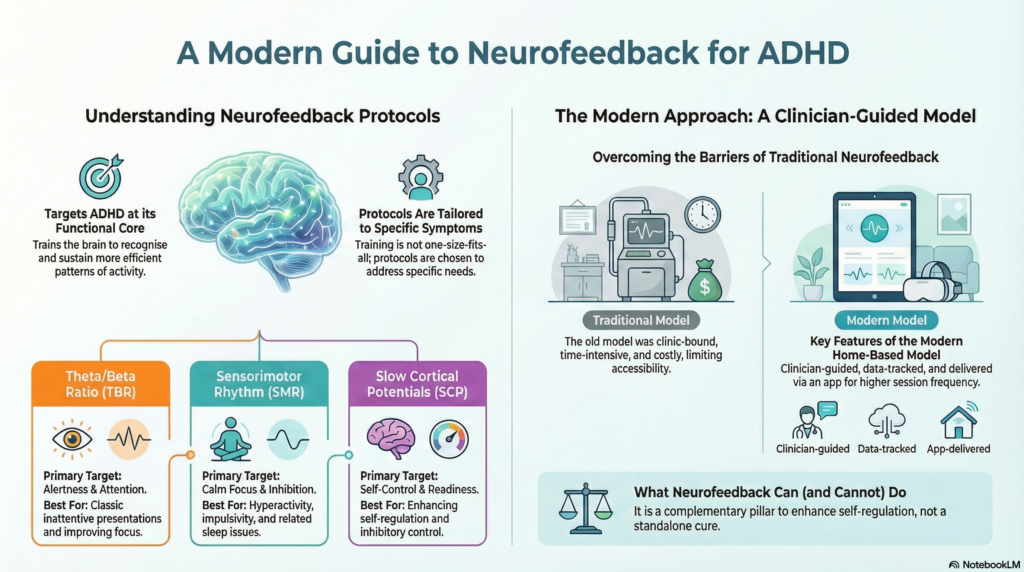
Neurofeedback targets the problem closer to its functional core:
training the brain to recognize and sustain more efficient patterns of activity.
From a decision-science perspective, neurofeedback does not replace clinical judgment. It adds a learning loop—something ADHD treatment often lacks once medication is started.
Commonly Used Neurofeedback Protocols in ADHD
1. Theta/Beta Ratio (TBR) Training
Historically, the most studied ADHD protocol.
-
ADHD populations—especially children—often show relatively increased theta (4–8 Hz) and reduced beta (13–20 Hz) activity.
-
TBR training reinforces reduction of excessive theta and enhancement of beta activity.
-
Clinically, this corresponds to improved alertness and sustained attention.
Strengths:
Well-studied, intuitive, useful in classic inattentive presentations.
Limitations:
Not all ADHD patients show elevated TBR. Blind application without EEG guidance can be ineffective.
2. Sensorimotor Rhythm (SMR) Training (12–15 Hz)
SMR protocols aim to enhance calm, focused motor-cortical states.
-
Often useful when hyperactivity, impulsivity, or motor restlessness is prominent.
-
May indirectly improve sleep and behavioral inhibition.
Strengths:
Good tolerability, useful in combined ADHD and sleep dysregulation.
Limitations:
Less specific to attentional networks alone.
3. Slow Cortical Potentials (SCP) Training
SCP neurofeedback trains regulation of very slow shifts in cortical excitability.
-
Focuses on readiness, inhibition, and self-control rather than frequency bands.
-
Requires more cognitive engagement and structured training.
Strengths:
Strong evidence in pediatric ADHD, durable effects.
Limitations:
Technically demanding, harder to deliver outside specialized centers.
What the Evidence Actually Says
The neurofeedback literature in ADHD is extensive but heterogeneous.
Broadly:
-
Children and adolescents show moderate, clinically meaningful improvements in core ADHD symptoms.
-
Sustained effects beyond the training period have been reported in several trials.
-
Adult ADHD data are promising but less robust, likely reflecting heterogeneity rather than inefficacy.
A key finding across studies:
Neurofeedback performs best when protocols are standardized and individualized, not symptom-matched blindly.
In other words, neurofeedback fails when treated as a generic intervention—and succeeds when treated as guided learning.
Where QEEG Fits In
QEEG is not required for all neurofeedback—but it improves decision quality.
It helps answer questions clinicians face daily:
-
Is this inattentiveness neurophysiological or affective?
-
Which networks appear under- or over-regulated?
-
Which protocol is likely to be inefficient or counterproductive?
Used properly, QEEG does not “diagnose ADHD.”
It constrains uncertainty, allowing more targeted training.
The Myndlift-Based Model: Neurofeedback Beyond the Clinic
Traditional neurofeedback is clinic-bound, time-intensive, and resource heavy. This limits accessibility and adherence—especially in adults with ADHD.
Myndlift represents a newer model:
-
clinician-guided
-
home-based
-
data-tracked
-
protocol-driven
How Myndlift Works in ADHD Practice
-
Initial EEG assessment and clinical intake guide protocol selection
-
Training sessions are delivered via an app using validated EEG headsets
-
Progress is monitored remotely by the clinician
-
Protocols are adjusted based on symptom response and EEG trends
This shifts neurofeedback from a procedure to a process.
Clinical Advantages of the Myndlift Model
-
Improves accessibility and adherence
-
Allows higher session frequency without clinic overload
-
Encourages patient engagement and agency
-
Generates longitudinal data rather than episodic impressions
Most importantly, it fits ADHD reality:
a disorder where consistency matters more than intensity.
What Neurofeedback Can—and Cannot—Do
Neurofeedback is not:
-
a replacement for medication in all cases
-
a shortcut to avoid behavioral work
-
a standalone cure
But it can:
-
improve attentional control
-
reduce reliance on escalating medication doses
-
enhance self-regulation skills
-
offer an objective training pathway for motivated patients
Used well, it becomes a complementary pillar, not a competing ideology.
A Clinician’s Perspective
From a Druckerian lens, ADHD care is decision-making under uncertainty. Neurofeedback adds feedback to that system.
Not certainty.
Not guarantees.
But learning.
And learning—whether in brains or organizations—is what leads to durable change.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Dr. Srinivas practices at Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall), Chennai, with a focused interest in adult ADHD, objective assessment (QEEG, CPT), neurofeedback-informed treatment planning, and home-based neurofeedback models including Myndlift. His clinical approach integrates psychiatry, neuroscience, and decision science.
📍 Apollo Clinic Velachery, Chennai
📞 +91-8595155808
✉️ srinivasaiims@gmail.com
🌐 https://srinivasaiims.com