SSRIs, Withdrawal, and Internet Misinformation: What Science Actually Tells Us
 Selective serotonin reuptake inhibitors (SSRIs) are among the most commonly prescribed medications in psychiatry. They have helped millions recover from depression, anxiety, panic disorder, OCD, and trauma-related conditions.
Selective serotonin reuptake inhibitors (SSRIs) are among the most commonly prescribed medications in psychiatry. They have helped millions recover from depression, anxiety, panic disorder, OCD, and trauma-related conditions.
Yet online, a very different narrative dominates. Social media is saturated with emotionally charged claims: “SSRIs permanently damaged my brain,” “Doctors never warned us,” “Withdrawal is worse than the illness,” “These drugs numb your emotions forever.”
Some of these stories describe genuine suffering. Others oversimplify complex neurobiology into moral outrage. The problem is not that patients are asking questions—the problem is that algorithm-driven misinformation collapses nuance into fear.
This article aims to clarify what we actually know about SSRI withdrawal, emotional numbing, and long-term effects—without denial, minimisation, or alarmism.
SSRI Withdrawal Is Real — but It Is Not Just “Bad Tapering”
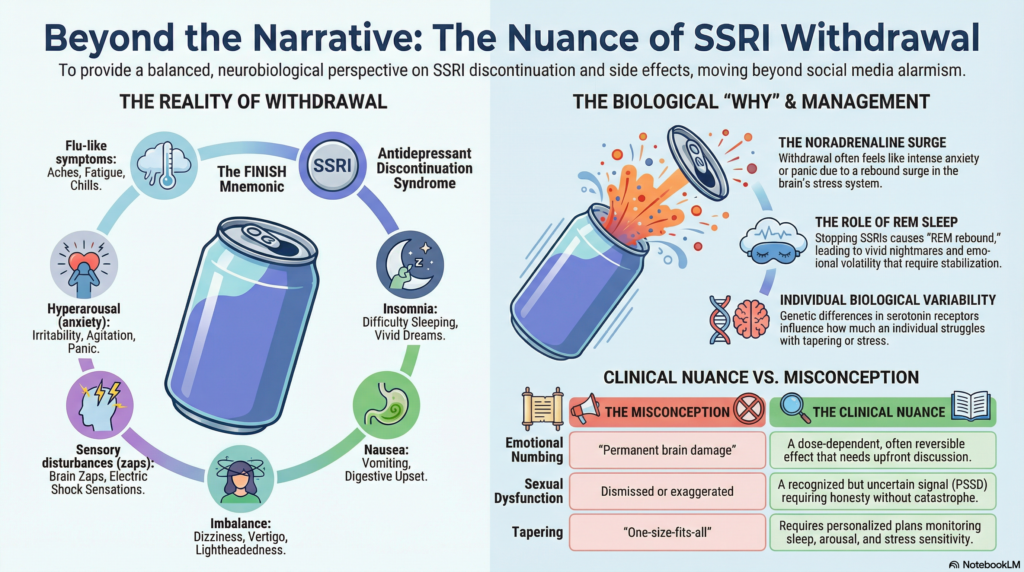
Stopping SSRIs can produce a cluster of symptoms collectively known as antidepressant discontinuation syndrome. These symptoms can be distressing and, in some individuals, severe.
Commonly reported features are captured by the FINISH mnemonic:
-
Flu-like symptoms
-
Insomnia and vivid dreams
-
Nausea
-
Imbalance and dizziness
-
Sensory disturbances (tingling, “electric shock” sensations)
-
Hyperarousal (anxiety, irritability, agitation)
What is often missed in online discussions is why these symptoms occur. Withdrawal is frequently framed as a simple “serotonin deficit.” That explanation is incomplete.
Neuroscience shows that SSRIs modulate multiple interconnected systems, not serotonin alone.
The Overlooked Player: Noradrenaline and the Stress System
SSRIs dampen activity in the locus coeruleus, the brain’s primary source of noradrenaline (norepinephrine). This indirectly calms the amygdala, reducing hyperarousal, fear, panic, and stress reactivity.
When SSRIs are stopped—especially abruptly—this inhibitory effect is removed. The result, in some individuals, is a rebound surge of noradrenergic activity.
This explains why withdrawal often feels less like “low mood” and more like:
-
intense anxiety or panic
-
agitation and irritability
-
insomnia and nightmares
-
sensory hypersensitivity
-
autonomic symptoms (sweating, palpitations, dizziness)
In simple terms:
SSRIs act like a lid on a shaken soda can. Sudden removal lets the pressure explode outward.
This mechanism is well described in neurobiological models of withdrawal and explains why symptoms often resemble hyperarousal rather than depression itself .
Why Sleep Matters More Than Most People Realise
SSRIs suppress REM sleep. When they are stopped, REM rebound occurs.
REM sleep is normally associated with a phenomenon called noradrenergic “time-out”—a pause that allows emotional processing and neural recalibration. During withdrawal, this pause may be lost due to noradrenaline excess, resulting in:
-
vivid dreams
-
nightmares
-
fragmented sleep
-
emotional volatility the following day
Sleep disruption then further amplifies noradrenergic activity, creating a self-reinforcing loop.
This is why early withdrawal management must prioritise sleep stabilisation, not just dose reduction.
Why Some People Struggle Much More Than Others
A critical but rarely discussed fact: people are biologically different.
Research suggests that individual variability in serotonin-1A (5-HT1A) receptor function, including genetic polymorphisms, may influence:
-
stress sensitivity
-
emotional regulation
-
vulnerability to withdrawal symptoms
These receptors play a role in:
-
neuronal excitability
-
anxiety regulation
-
resilience to stress
For some individuals, stopping an SSRI represents a major allostatic load—a stressor that overwhelms the brain’s capacity to return to equilibrium. In such cases, symptoms may become prolonged not because of “damage,” but because stress systems have become sensitised.
This helps explain why:
-
hyperbolic tapering works well for many
-
but worsens symptoms in a subset
-
and why re-introducing medication can sometimes intensify distress instead of relieving it
Biology matters. Context matters. Labels alone do not.
Emotional Numbing: A Side Effect That Deserves Honesty
Emotional blunting is a recognised SSRI effect in some patients. It is:
-
dose-dependent
-
often reversible
-
sometimes helpful early in severe depression or anxiety
-
problematic when left unaddressed long-term
The mistake has been under-discussing this effect, not exaggerating it. When patients feel emotionally flattened and were never warned, trust erodes—and online narratives rush in to fill the gap.
Transparent discussion upfront prevents resentment later.
Post-SSRI Sexual Dysfunction (PSSD): Signal, Uncertainty, and Responsibility
Persistent sexual dysfunction after SSRI exposure has been reported. It should not be dismissed.
At the same time:
-
the true prevalence is unknown
-
mechanisms are not clearly established
-
causality is often inferred retrospectively
Responsible psychiatry sits between denial and catastrophe. Patients deserve acknowledgement of uncertainty, not false reassurance or fear-based certainty.
Why Internet Ragebait Feels Convincing (and Why It Misleads)
Social media amplifies:
-
emotional intensity
-
moral framing
-
personal testimony without denominator data
Once people are distressed, their brains—understandably—seek meaning. A single explanation (“the drug broke me”) is psychologically simpler than navigating relapse risk, withdrawal physiology, stress sensitisation, and uncertainty.
But simple stories are not always accurate stories.
What Good Psychiatric Practice Looks Like Today
Modern, ethical SSRI prescribing includes:
-
explicit discussion of sexual and emotional side effects
-
tapering education before starting treatment
-
personalised discontinuation plans
-
monitoring sleep, arousal, and stress sensitivity
-
avoiding rigid one-size-fits-all tapering dogma
Most importantly, it involves listening without defensiveness.
Validation does not mean blame. Understanding does not mean dismissal.
The Bottom Line
SSRIs are not “chemical lobotomies.”
They are not harmless vitamins either.
They are powerful neurobiological tools used in complex human systems shaped by biology, stress, trauma, expectations, and meaning.
Internet misinformation thrives on certainty. Psychiatry must survive on careful thinking, transparency, and humility.
The goal is not to silence criticism—but to replace fear with understanding, and outrage with literacy.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall), Chennai
Dr. Srinivas specialises in mood disorders, anxiety, sleep disorders, medication optimisation, and neurobiologically informed psychiatry. He regularly writes and speaks on psychopharmacology, withdrawal phenomena, and ethical mental health practice in the digital age.
✉ srinivasaiims@gmail.com
📞 +91-8595155808