Paracetamol in Pregnancy and Autism: Separating Evidence from Internet Panic
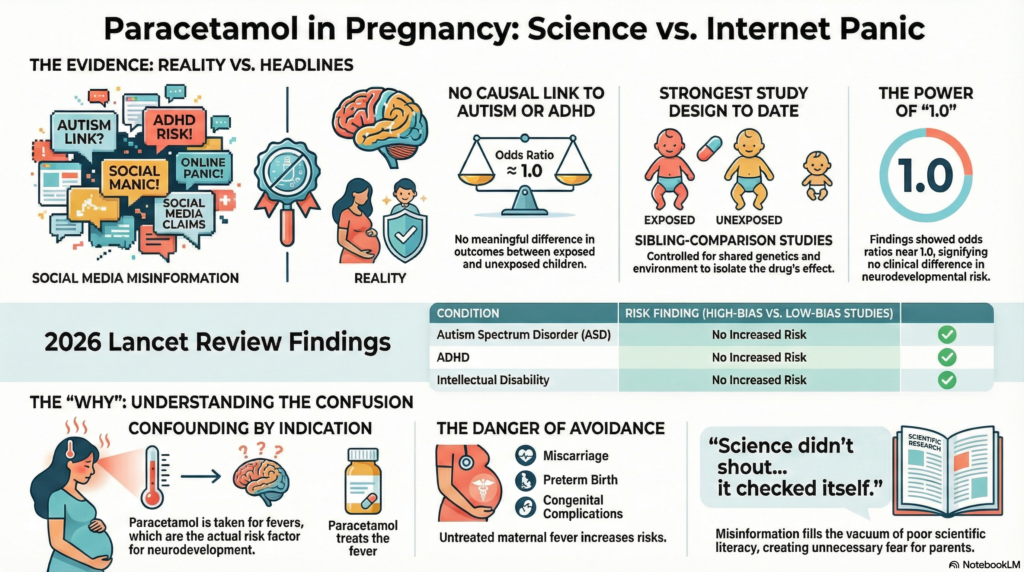
Few medical topics ignite online anxiety as reliably as pregnancy and autism. Add a common medicine like paracetamol (acetaminophen) to the mix, and you get a perfect storm of fear, headlines, and half-digested science. Over the past year, social media has been flooded with claims that “paracetamol causes autism.”
Science, however, has a stubborn habit of being less dramatic—and far more careful.
A large systematic review and meta-analysis published in The Lancet Obstetrics, Gynaecology & Women’s Health (January 2026) finally gives us the clarity that public discourse has lacked.
Let’s walk through what this study actually tells us, and why it matters.
Why This Question Even Came Up
Paracetamol is the most commonly used pain-reliever and fever medication during pregnancy, recommended worldwide because alternatives like NSAIDs and opioids carry clearer risks.
Earlier observational studies reported small associations between prenatal paracetamol exposure and later diagnoses such as:
-
Autism spectrum disorder (ASD)
-
ADHD
-
Intellectual disability
These studies were widely circulated—often without context—and quickly weaponised online. But association is not causation. Pregnancy itself is biologically noisy territory: fever, infection, pain, inflammation, genetics, and family environment all tangle together.
The real question was never “Did some studies show a signal?”
It was: Does paracetamol itself cause neurodevelopmental disorders once we control properly for confounders?
What Makes This Lancet Study Different
This paper didn’t just pool studies and average numbers. It ranked evidence by methodological strength.
The authors prioritised sibling-comparison studies—a powerful design where siblings born to the same parents are compared, one exposed to paracetamol in utero and the other not. This approach controls for:
-
Shared genetics
-
Family environment
-
Socioeconomic background
-
Many unmeasured parental factors
In other words, it asks: within the same family, does paracetamol exposure change outcomes?
That’s as close as observational research gets to answering causal questions.
The Headline Findings (Spoiler: Reassuring)
Across the strongest analyses:
-
Autism spectrum disorder: No increased risk
-
ADHD: No increased risk
-
Intellectual disability: No increased risk
This held true when the authors:
-
Looked only at sibling-comparison studies
-
Restricted analysis to low-bias studies
-
Considered long-term follow-up (>5 years)
The odds ratios hovered around 1.0, meaning no meaningful difference between exposed and unexposed children .
If paracetamol had a clinically important neurodevelopmental effect, this is exactly the kind of analysis where it should have shown up. It didn’t.
So Why Did Earlier Studies Look Scary?
Because confounding by indication is a real beast.
Paracetamol isn’t taken randomly. It’s taken when mothers have:
-
Fever
-
Infection
-
Pain
-
Inflammatory states
Ironically, untreated maternal fever itself is a known risk factor for adverse pregnancy and neurodevelopmental outcomes. When studies don’t adequately separate the reason for taking the drug from the drug itself, paracetamol becomes the scapegoat.
Sibling-comparison designs neatly defang this problem—and when they do, the association disappears.
Biology vs Reality
Yes, paracetamol crosses the placenta.
Yes, theoretical mechanisms exist—oxidative stress, prostaglandin modulation, endocrine pathways.
But plausible mechanisms are not proof. Much of this mechanistic work comes from animal or in-vitro models at doses and conditions far removed from real-world clinical use. Human data, when rigorously analysed, simply do not support a causal link.
The Real Risk: Fear-Driven Avoidance
Here’s the uncomfortable irony.
Avoiding paracetamol during pregnancy based on misinformation can:
-
Leave maternal fever untreated
-
Increase risk of miscarriage, preterm birth, and congenital complications
-
Push patients toward less safe alternatives
This is why professional bodies worldwide—including obstetric and fetal-medicine societies—continue to recommend paracetamol as first-line therapy in pregnancy when used appropriately.
The Lancet paper doesn’t challenge that guidance. It reinforces it.
A Broader Lesson for Mental Health and Medicine
This episode is a case study in how:
-
Preliminary associations become viral “truths”
-
Nuanced science loses the algorithmic fight
-
Anxiety fills the vacuum left by poor scientific literacy
As clinicians, our job isn’t just to prescribe—it’s to interpret evidence, contextualise risk, and prevent harm caused by misinformation.
Final Take-Home
-
The best available evidence does not support a causal link between prenatal paracetamol use and autism, ADHD, or intellectual disability
-
Earlier alarming signals are best explained by confounding, not toxicity
-
Fear-based avoidance may do more harm than good
Science didn’t shout. It did something better—it checked itself.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
I work at the intersection of psychiatry, neuroscience, and evidence-based medicine, with a special interest in separating real risk from manufactured panic—especially in areas like neurodevelopment, medications, and public mental health narratives.
✉ srinivasaiims@gmail.com
📞 +91-8595155808
Thoughtful medicine begins where fear ends.