Why Are Antipsychotic Medicines Increasingly Used in Older Adults?
 If you or a loved one is above 60 and has been prescribed medicines like quetiapine, risperidone, olanzapine, or haloperidol, you may naturally wonder:
If you or a loved one is above 60 and has been prescribed medicines like quetiapine, risperidone, olanzapine, or haloperidol, you may naturally wonder:
-
Is this common?
-
Is it safe?
-
Why are these medicines being used more often now?
Recent large-scale research from the United States gives us some important clues—and also helps us understand broader global trends that are relevant to India as well.
Let’s break this down calmly and clearly.
First, what do the numbers say?
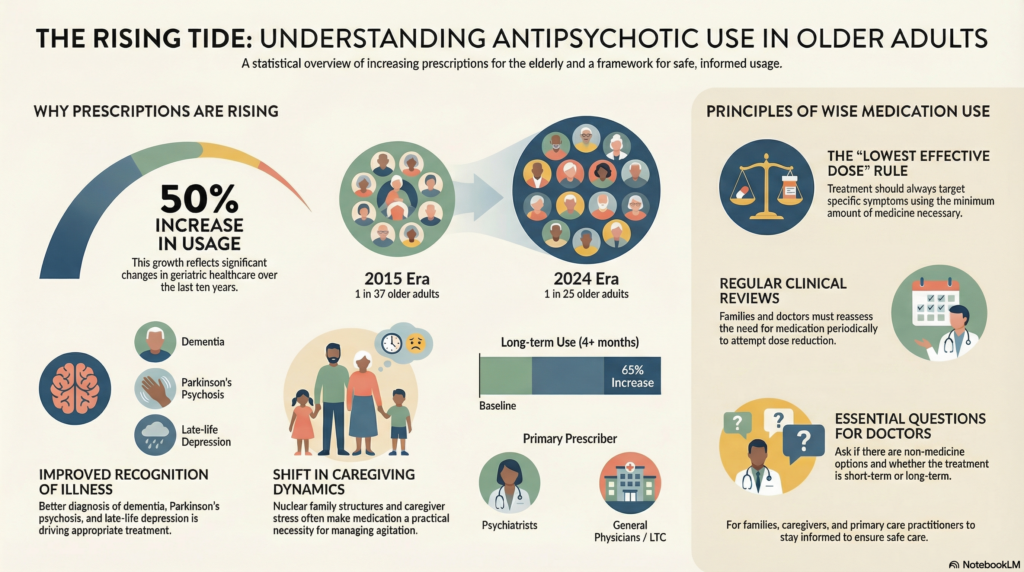
Between 2015 and 2024, the use of antipsychotic medications in adults aged 65 years and above increased by more than 50%.
-
Earlier: about 1 in 37 older adults used an antipsychotic in a year
-
Now: about 1 in 25 older adults do
Even more important:
-
Long-term use (4 months or more per year) increased by nearly 65%
So yes—these medicines are being used more often, and for longer durations, in elderly people.
Does this mean doctors are “over-prescribing”?
The answer is more nuanced than a simple yes or no.
Several interacting reasons explain this rise.
1. Better recognition of psychiatric illness in the elderly
One positive change is improved awareness.
Earlier generations often dismissed symptoms as:
-
“Old age behaviour”
-
“Stubbornness”
-
“Just memory loss”
Today, doctors are better at diagnosing:
-
Dementia and behavioural symptoms
-
Late-life depression
-
Psychosis in Parkinson’s disease
-
Mood disorders presenting for the first time after 60
As diagnosis improves, treatment naturally increases.
This reflects progress—not necessarily excess.
2. Behavioural symptoms in dementia are increasing
People are living longer, and with longer life comes:
-
Alzheimer’s disease
-
Vascular dementia
-
Mixed cognitive disorders
Many dementia patients develop:
-
Agitation
-
Aggression
-
Suspiciousness
-
Night-time restlessness
-
Hallucinations or fearfulness
These symptoms can be distressing for families and difficult to manage without support.
In real-world settings—especially where trained caregivers or behavioural therapy is limited—medicines are often used as a practical solution.
3. Sleep problems in older adults are a major driver
This is one of the most under-recognised reasons.
As people age:
-
Sleep becomes lighter
-
Night awakenings increase
-
Circadian rhythm shifts earlier
-
Medical illnesses disturb sleep
Many older adults suffer from:
-
Chronic insomnia
-
Night-time confusion
-
Sundowning symptoms
Low-dose antipsychotics (especially quetiapine) are sometimes prescribed off-label for sleep, particularly when:
-
Benzodiazepines are avoided
-
Melatonin fails
-
There is associated anxiety or confusion
This practice partly explains the rising numbers.
4. Shift in family structure and caregiving stress
Earlier, joint families absorbed behavioural difficulties.
Today:
-
Nuclear families are common
-
Caregivers are working
-
Elderly may live alone or in assisted facilities
When agitation, paranoia, or night-time disturbances disrupt daily life, families understandably seek fast relief.
Medication becomes the easiest accessible tool.
5. More prescriptions are coming from non-psychiatrists
Interestingly, research shows:
-
Prescriptions from psychiatrists have reduced
-
Prescriptions from general physicians and long-term care settings have increased
This does not imply poor care—but reflects reality:
-
Psychiatrists are fewer
-
Primary doctors manage most elderly patients
-
Follow-up time is limited
In such settings, medicines that “settle symptoms” tend to be preferred over complex non-drug strategies.
6. Decline in older antipsychotics, rise of newer ones
There is some good news.
Use of older antipsychotics (like haloperidol) has reduced.
Doctors are now more likely to use newer medications, which are generally:
-
Better tolerated
-
Less likely to cause severe movement disorders
This shows improving prescribing quality—even as overall use rises.
Should patients and families be worried?
Not automatically.
Antipsychotic medicines:
-
Do have a role
-
Can be very helpful in selected situations
-
Should not be demonised
But they must be used thoughtfully, especially in older adults.
Key principles matter:
-
Lowest effective dose
-
Clear target symptoms
-
Regular review
-
Attempts to reduce or stop when possible
What should families ask their doctor?
Simple, respectful questions help ensure safe care:
-
What symptoms are we treating?
-
Is this medicine short-term or long-term?
-
Are there non-medicine options we should try?
-
How will we review side effects?
-
When will we reassess the need?
Good psychiatry is not about avoiding medicines—
it is about using them wisely.
The bigger picture
The rising use of antipsychotics in older adults reflects:
-
Better diagnosis
-
Longer life expectancy
-
More dementia-related symptoms
-
Sleep disturbances
-
Caregiver stress
-
System-level limitations
The solution is not fear—but balanced, informed care.
As populations age, mental health support for the elderly must grow not just in prescriptions—but in time, counselling, caregiver education, and follow-up.
That is the direction ethical psychiatry must take.
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
✉ srinivasaiims@gmail.com 📞 +91-8595155808