AuDHD in Adults: Burnout, Masking, and Late Diagnosis
 A research-informed clinical guide to an under-recognised reality
A research-informed clinical guide to an under-recognised reality
Many adults arrive in mental health clinics with a familiar story:
“I’ve always managed somehow… until I suddenly couldn’t.”
They describe chronic exhaustion, loss of skills, emotional volatility, declining tolerance for people or noise, and a sense that life has become unmanageably heavy. They are often diagnosed—again—with anxiety or depression. Medications help a little, then stop helping. Therapy feels effortful but oddly missing the point.
For a growing number of these adults, the missing framework is AuDHD: the co-occurrence of Autism Spectrum traits and ADHD traits in the same individual.
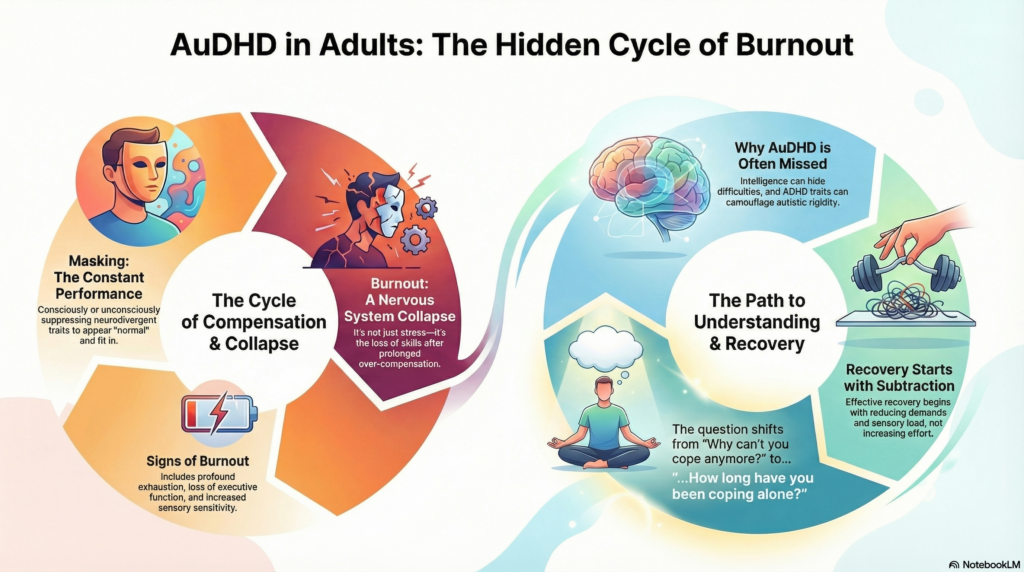
This article focuses on three defining features of adult AuDHD:
-
Masking
-
Burnout
-
Late or missed diagnosis
1. Why AuDHD is frequently missed in adulthood
Until relatively recently, diagnostic systems did not formally allow a dual diagnosis of autism and ADHD. This changed with DSM-5, but clinical habits lag behind manuals.
In adults, AuDHD is often missed because:
-
Intelligence and verbal ability mask developmental difficulties
-
Academic success creates a false sense of “functioning”
-
ADHD traits camouflage autistic rigidity
-
Autistic structure compensates for ADHD impulsivity
-
Symptoms are interpreted through a psychiatric lens rather than a neurodevelopmental one
The result is partial diagnosis: ADHD without autism, or “anxiety” without recognising the neurodevelopmental substrate.
2. Masking: the hidden labour of AuDHD adults
What is masking?
Masking refers to the conscious or unconscious suppression of natural neurodivergent traits in order to appear “normal”.
In adults with AuDHD, masking often includes:
-
Forcing eye contact
-
Scripted social responses
-
Suppressing stimming or sensory avoidance
-
Over-preparing for conversations
-
Mimicking peers
-
Excessive self-monitoring
-
Intellectualising emotions
Masking is not deception.
It is adaptive survival.
Why AuDHD adults mask more intensely
ADHD brings social impulsivity and novelty-seeking; autism brings social uncertainty and sensory sensitivity. Together, they create a powerful drive to fit in while constantly feeling out of sync.
Adults with AuDHD often:
-
Learn early that authenticity leads to rejection
-
Become highly socially skilled—but at great internal cost
-
Appear confident while feeling chronically unsafe
Masking works—until it doesn’t.
3. Burnout: when compensation collapses
What is autistic / neurodivergent burnout?
Burnout in AuDHD is not ordinary stress. It is a state of nervous-system collapse following prolonged over-compensation.
Common features include:
-
Profound physical and mental exhaustion
-
Loss of executive function
-
Reduced speech or social capacity
-
Increased sensory sensitivity
-
Emotional blunting or shutdown
-
Increased meltdowns or withdrawal
-
Reduced tolerance to work, relationships, or parenting
Crucially, burnout involves loss of previously available skills, not just low mood.
Why burnout often occurs in adulthood
Many AuDHD adults cope well until:
-
Work demands increase
-
Parenting responsibilities begin
-
Support structures disappear
-
Chronic sleep deprivation sets in
-
Sensory and social load becomes relentless
The nervous system reaches its limit.
This is often misdiagnosed as:
-
Major depressive disorder
-
Bipolar disorder
-
Personality disorder
-
“Treatment-resistant” anxiety or depression
The underlying issue is allostatic overload—years of adaptation without recovery.
4. Late diagnosis: why it feels both relieving and destabilising
Receiving an AuDHD formulation in adulthood can provoke mixed emotions:
-
Relief (“There’s an explanation.”)
-
Grief (“What if I’d known earlier?”)
-
Anger (“Why was this missed?”)
-
Fear (“Who am I without the mask?”)
Late diagnosis challenges deeply held self-narratives built around:
-
Laziness
-
Failure
-
Emotional instability
-
Being “too much” or “not enough”
For many adults, diagnosis is not the end point—it is the beginning of unlearning.
5. Clinical features that suggest AuDHD in adults
AuDHD should be considered when adults show:
-
Longstanding executive dysfunction with sensory sensitivity
-
Social exhaustion despite apparent competence
-
Alternation between rigid routines and impulsive novelty-seeking
-
Chronic burnout despite intelligence and effort
-
Partial response to ADHD medication
-
Anxiety or mood symptoms that fluctuate with overload
-
A lifelong sense of being “out of sync”
Developmental history remains essential—even when childhood seemed “successful”.
6. Treatment principles: why standard approaches often fail
Medication
Stimulants may improve focus, but:
-
Sensory sensitivity may increase
-
Anxiety may transiently worsen
-
Burnout does not resolve with stimulants alone
Medication addresses attention, not overload.
Therapy
Traditional CBT may struggle unless adapted.
Helpful adaptations include:
-
Neurodiversity-affirming CBT
-
Executive function coaching
-
Emotion regulation skills
-
Psychoeducation about masking and burnout
The aim is capacity-building, not symptom suppression.
Environment over effort
For AuDHD adults, design beats discipline.
Effective supports include:
-
Reduced sensory load
-
Predictable routines with flexible entry points
-
Clear boundaries around work hours
-
Structured rest (not just “vacations”)
-
Thoughtful screen and sleep hygiene
Recovery is subtractive before it is additive.
7. Recovery from burnout: what actually helps
Burnout recovery requires:
-
Validation (this is not weakness)
-
Reduced demands
-
Permission to unmask gradually
-
Rebuilding routines at lower intensity
-
Sensory regulation as daily maintenance
-
Time—often months, not weeks
Pushing through burnout prolongs it.
8. Reframing adult AuDHD
AuDHD is not a deficit identity.
It is a neurodevelopmental configuration that has survived through adaptation—often at high cost.
When supported, AuDHD adults often bring:
-
Original thinking
-
Pattern recognition
-
Empathy rooted in lived experience
-
Creativity and innovation
-
Deep ethical awareness
But strengths emerge only when the nervous system is no longer in survival mode.
Key take-home messages
-
Masking keeps AuDHD adults functioning—until it causes burnout
-
Burnout reflects system overload, not psychiatric failure
-
Late diagnosis is common and often transformative
-
Treatment must address regulation, not just productivity
-
Recovery begins with reducing demands, not increasing effort
The most helpful question is not:
“Why can’t you cope anymore?”
But:
“How long have you been coping alone?”
References
-
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: APA; 2013.
-
Leitner Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children – what do we know? Front Hum Neurosci. 2014;8:268.
-
Antshel KM, Russo N. Autism spectrum disorders and ADHD: overlapping phenomenology, diagnostic issues, and treatment considerations. Curr Psychiatry Rep. 2019;21(5):34.
-
Young S, Asherson P, Lloyd T, Absoud M, Arif M, Colley W, et al. Failure of healthcare provision for adults with ADHD and autism spectrum disorder. BMC Psychiatry. 2020;20:404.
-
Raymaker DM, Teo AR, Steckler NA, Lentz B, Scharer M, Delos Santos A, et al. “Having all of your internal resources exhausted beyond measure”: a qualitative study of autistic burnout. Autism Adults. 2020;2(2):132-143.
-
Cassidy S, Bradley L, Robinson J, Allison C, McHugh M, Baron-Cohen S. Suicidal ideation and suicide plans or attempts in adults with Asperger’s syndrome attending a specialist diagnostic clinic. Lancet Psychiatry. 2014;1(2):142-147.
About the author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist
Apollo Clinic Velachery (Opp. Phoenix Mall), Chennai
Dr. Srinivas works with adults and adolescents on ADHD, autism spectrum conditions, burnout, emotional regulation, and neurodevelopmental differences, integrating clinical psychiatry with neuroscience-informed, compassionate care.
✉ srinivasaiims@gmail.com
📞 +91-8595155808