AuDHD: Understanding the Overlap Between Autism and ADHD
 A clear, research-informed guide for parents, adults, and clinicians
A clear, research-informed guide for parents, adults, and clinicians
In recent years, a term has quietly entered clinical conversations, online communities, and lived-experience narratives: AuDHD.
It is not a diagnosis found in manuals. It is a descriptive shorthand used to capture something clinicians have always seen but often struggled to name clearly—the co-occurrence of Autism Spectrum traits and Attention-Deficit/Hyperactivity traits in the same individual.
AuDHD is not rare. It is under-recognised.
This article explains what AuDHD is, why it looks confusing in real life, how it differs from “pure” ADHD or autism, and what actually helps.
1. Why AuDHD matters (and why it was missed for so long)
Historically, diagnostic systems treated autism and ADHD as mutually exclusive. Earlier editions of DSM did not allow both diagnoses simultaneously. This changed only with DSM-5, which formally recognised that ADHD and autism can and do co-occur.
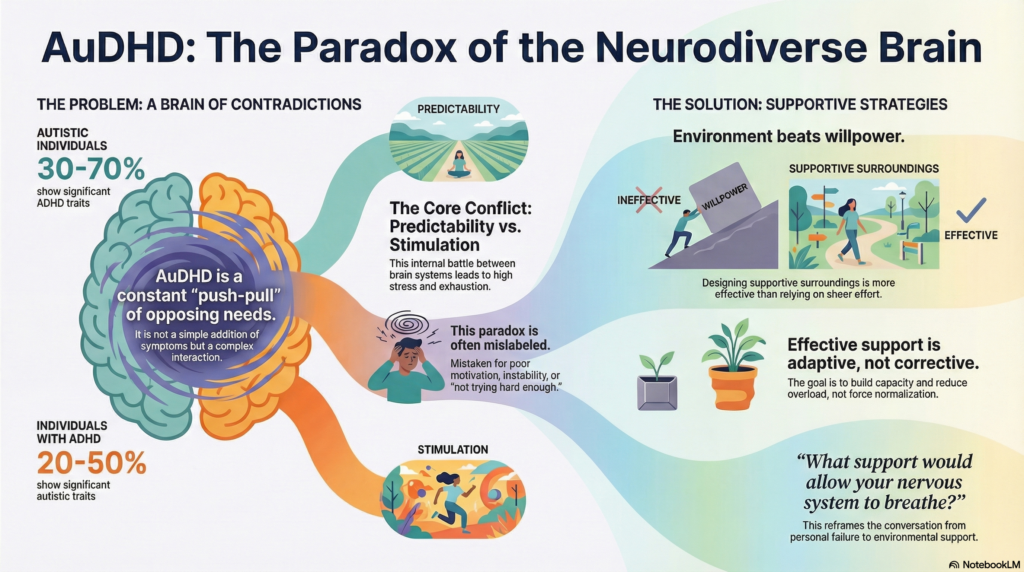
Research now consistently shows:
-
30–70% of autistic individuals show clinically significant ADHD traits
-
20–50% of individuals with ADHD show autistic traits
Yet many people—especially adolescents and adults—remain misdiagnosed or partially diagnosed.
Why?
Because AuDHD does not look like a simple addition of symptoms.
It looks like internal contradiction.
2. The paradox at the heart of AuDHD
People with AuDHD often describe living with opposing forces inside the same mind.
Common paradoxes include:
-
Craving structure but resisting routines
-
Needing predictability yet constantly seeking novelty
-
Hyperfocusing intensely, then burning out suddenly
-
Wanting social connection but finding it exhausting
-
Being highly sensitive yet appearing distractible or impulsive
This internal push-pull is often mistaken for:
-
Personality problems
-
Emotional instability
-
Poor motivation
-
“Not trying hard enough”
In reality, it reflects two neurodevelopmental profiles interacting, not canceling each other out.
3. A neurobiological lens: why AuDHD feels so hard
Autism and ADHD involve different—but overlapping—neural networks.
Very simply:
-
ADHD is strongly linked to differences in dopamine-mediated reward, attention regulation, and impulse control
-
Autism is linked to differences in sensory processing, social cognition, prediction, and cognitive flexibility
In AuDHD:
-
The ADHD brain seeks stimulation
-
The autistic brain seeks predictability
-
The nervous system oscillates between overload and under-stimulation
This produces high allostatic load—the brain is constantly adapting, recalibrating, and compensating.
That’s exhausting.
4. How AuDHD presents across the lifespan
In childhood
-
High intelligence with inconsistent performance
-
Sensory sensitivities plus impulsivity
-
Meltdowns that look “behavioral” but are sensory-emotional overload
-
Early school difficulties despite apparent ability
Often labelled as:
“naughty”, “lazy”, “oppositional”, or “over-sensitive”.
In adolescence
-
Emotional volatility
-
Academic underachievement despite potential
-
Social exhaustion
-
Increasing anxiety or low self-esteem
-
Heavy reliance on screens for regulation
Masking often increases here—especially in girls and gender-diverse adolescents.
In adulthood
-
Chronic burnout
-
Executive dysfunction
-
Difficulty sustaining routines
-
Career instability despite talent
-
Relationship misunderstandings
-
Late diagnoses after anxiety, depression, or “treatment resistance”
Many adults with AuDHD are diagnosed with ADHD first, and autism much later—if at all.
5. Why AuDHD is frequently misdiagnosed
AuDHD is often mistaken for:
-
Borderline personality traits
-
Bipolar spectrum conditions
-
Complex anxiety disorders
-
“Pure” ADHD with emotional dysregulation
The key difference:
In AuDHD, difficulties are developmental and lifelong, even if symptoms fluctuate.
Mood symptoms often arise secondarily, from chronic overload and repeated failure experiences.
6. Assessment: what good evaluation looks like
A proper AuDHD assessment is multidimensional, not checklist-based.
It should include:
-
Developmental history (early childhood matters)
-
Sensory profile
-
Attention and executive functioning
-
Social communication patterns
-
Emotional regulation strategies
-
Masking and compensation behaviours
Brief screenings alone are insufficient.
7. Treatment principles: why “one-size-fits-all” fails
Medication
Stimulants can help attention in AuDHD—but:
-
Sensory sensitivity may increase
-
Anxiety may transiently worsen
-
Dosing often needs to be lower and slower
Medication helps one axis, not the whole system.
Therapy
Standard CBT often needs adaptation.
Helpful approaches include:
-
Neurodiversity-affirming CBT
-
Skills-based executive function coaching
-
Emotion regulation training
-
Psychoeducation (this alone can be transformative)
The goal is capacity-building, not normalization.
Environment beats effort
For AuDHD, design matters more than motivation.
Helpful strategies:
-
External structure without rigidity
-
Predictable routines with flexible entry points
-
Sensory regulation built into daily life
-
Reduced cognitive load
-
Clear boundaries around screens and sleep
Willpower is unreliable when the nervous system is overloaded.
8. AuDHD and burnout: an important warning
Many adults with AuDHD present only after burnout.
Burnout signs include:
-
Loss of skills
-
Reduced tolerance to noise/social interaction
-
Increased shutdowns or meltdowns
-
Cognitive fog
-
Emotional blunting
Burnout is not laziness.
It is system collapse after prolonged compensation.
Recovery requires:
-
Rest
-
Reduced expectations
-
Validation
-
Gradual rebuilding—not pushing harder.
9. Reframing AuDHD: from deficit to difference
AuDHD minds often bring:
-
Original thinking
-
Deep curiosity
-
Pattern recognition
-
Creativity
-
Empathy rooted in lived struggle
But these strengths emerge only when the nervous system is supported.
Understanding AuDHD is not about labels.
It is about reducing shame and building environments where people can function without constant self-override.
The take-home message
AuDHD is not a trend.
It is a long-ignored reality.
When autism and ADHD coexist, support must be:
-
Developmentally informed
-
Sensory-aware
-
Structurally intelligent
-
Compassionate rather than corrective
The question is not:
“Why can’t you be consistent?”
The better question is:
“What support would allow your nervous system to breathe?”
References
-
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: APA; 2013.
-
Leitner Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children – what do we know? Front Hum Neurosci. 2014;8:268.
-
Antshel KM, Russo N. Autism spectrum disorders and ADHD: overlapping phenomenology, diagnostic issues, and treatment considerations. Curr Psychiatry Rep. 2019;21(5):34.
-
Craig F, et al. A review of executive function deficits in autism spectrum disorder and ADHD. Neuropsychiatr Dis Treat. 2016;12:1191–1202.
-
Young S, et al. ADHD and autism spectrum disorder in adults: clinical implications of a dimensional approach. BMC Psychiatry. 2020;20:404.
About the author
Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi)
Consultant Psychiatrist
Apollo Clinic Velachery (Opp. Phoenix Mall), Chennai
Dr. Srinivas works with children, adolescents, and adults on ADHD, autism spectrum conditions, emotional regulation, and neurodevelopmental differences, integrating clinical psychiatry with neuroscience-informed, practical care.
✉ srinivasaiims@gmail.com
📞 +91-8595155808