Bupropion-Dextromethorphan Combination for Depression: A Comprehensive Review
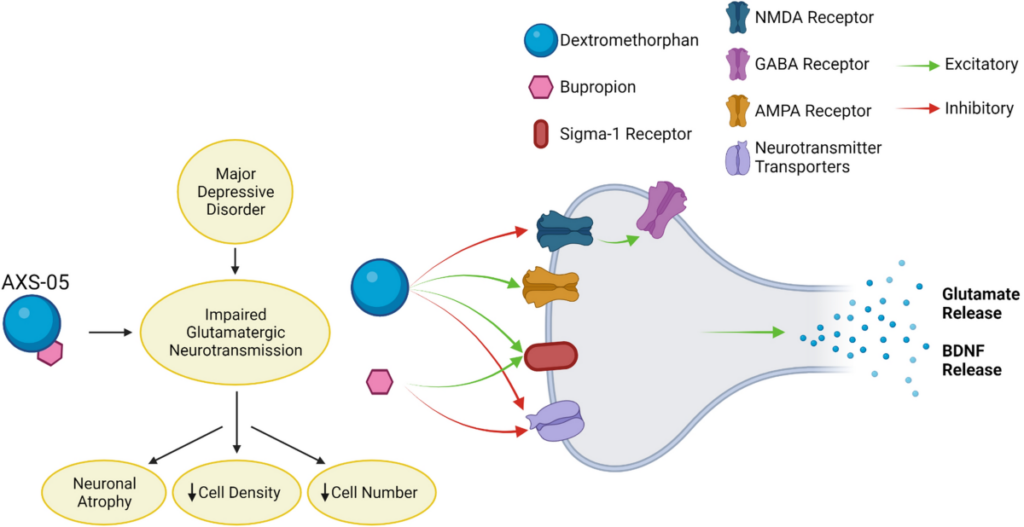
The combination of bupropion and dextromethorphan (marketed as Auvelity in the U.S.) represents a groundbreaking pharmacological approach to treating major depressive disorder (MDD). It offers a dual mechanism targeting both glutamatergic and monoaminergic systems, which are critical in depression. This review provides a detailed analysis of the evidence supporting its efficacy and safety.
Pharmacological Insights
1. Bupropion:
Classified as a norepinephrine-dopamine reuptake inhibitor (NDRI).
Improves symptoms of anhedonia and low energy often resistant to treatment with serotonin-targeted antidepressants.
2. Dextromethorphan:
Functions as an N-methyl-D-aspartate (NMDA) receptor antagonist, similar to ketamine but less dissociative.
Acts as a sigma-1 receptor agonist, enhancing intracellular signaling and neuronal survival mechanisms.
3. Synergistic Action:
Bupropion inhibits CYP2D6, the enzyme responsible for dextromethorphan metabolism, enhancing its bioavailability and therapeutic effects.
Together, they modulate glutamate and dopamine pathways, critical for rapid antidepressant effects.
Clinical Evidence
1. Randomized Controlled Trials (RCTs)
GEMINI Trial:
A pivotal 8-week, double-blind, placebo-controlled study of 327 adult patients with MDD.
Significant improvement in the Montgomery-Åsberg Depression Rating Scale (MADRS) scores by week 1 compared to placebo.
Demonstrated greater efficacy than traditional antidepressants in terms of speed and robustness.
ASCEND Trial:
Evaluated the combination in treatment-resistant depression (TRD).
Patients previously unresponsive to SSRIs/SNRIs achieved significant symptom relief within weeks, with sustained remission observed in 20-30% of participants.
2. Real-World Evidence
Early observational studies suggest that the combination is particularly effective in addressing anhedonia and cognitive symptoms of depression.
Patients report improved functionality and reduced suicidal ideation, which are often inadequately addressed by conventional antidepressants.
Advantages Over Traditional Antidepressants
1. Rapid Onset of Action:
Onset within 1 week, compared to 4-6 weeks for SSRIs/SNRIs.
Potential to reduce depressive episodes and improve quality of life more quickly.
2. Novel Mechanism:
Addresses treatment resistance by targeting glutamate pathways, an area of interest in the pathophysiology of MDD.
3. Improved Side Effect Profile:
Lower incidence of weight gain, sexual dysfunction, and sedation compared to SSRIs/SNRIs.
Potential Limitations
1. Long-Term Efficacy:
While short-term benefits are well-documented, more studies are needed to confirm long-term outcomes.
2. Adverse Effects:
Common side effects include nausea, dizziness, and dry mouth.
Risk of serotonin syndrome when combined with serotonergic drugs.
3. Cost and Accessibility:
As a novel therapy, it may be more expensive than generic antidepressants.
Patient-Centered Outcomes
Patients with treatment-resistant depression or those who experience significant cognitive impairments may particularly benefit from this combination. Anecdotal and trial data highlight improvements in:
Motivation and energy levels.
Social functioning.
Reduction in suicidal ideation.
Clinical Recommendations
1. Indications:
Approved for major depressive disorder and under investigation for other conditions like anxiety and post-traumatic stress disorder (PTSD).
Particularly beneficial for patients with treatment-resistant depression.
2. Dosing:
Administered as a fixed-dose combination with close monitoring for dose adjustments.
3. Monitoring:
Regular assessment of blood pressure and heart rate is necessary due to bupropion’s mild sympathomimetic effects.
Conclusion
The bupropion-dextromethorphan combination is a significant advance in depression treatment, particularly for patients who fail to respond to traditional therapies. By combining rapid-onset NMDA receptor antagonism with monoaminergic activity, it offers hope for a faster, more effective treatment with fewer side effects. As more studies emerge, it may redefine the standard of care for major depressive disorder.
Further research into its long-term effects and utility in comorbid psychiatric conditions could solidify its position as a cornerstone of depression pharmacotherapy.