Escitalopram FAQ
 Escitalopram was approved for medical use in the United States in 2002 and has since become one of the most widely prescribed antidepressants worldwide. It was developed as the active S-enantiomer of citalopram, allowing similar or better clinical benefits at lower doses, with improved tolerability and safety. Because of this, escitalopram is generally preferred over simply doubling the dose of citalopram. Its clinical importance is reflected in its inclusion on the World Health Organization’s List of Essential Medicines, a designation reserved for treatments considered effective, safe, and necessary for public health. By 2023, escitalopram had become the second most prescribed antidepressant and one of the most commonly prescribed medications overall in the United States, with tens of millions of prescriptions annually. Similar trends are seen globally, including Australia, where it has consistently ranked among the top prescribed medicines in recent years. In India, escitalopram is widely used in everyday psychiatric practice and is available under several familiar brand names such as Nexito, Cipralex, Escita, Zetalo, and others. While brand names may differ, the active medicine is the same, and treatment outcomes depend far more on correct dosing, consistency, and individual response than on the specific brand chosen.
Escitalopram was approved for medical use in the United States in 2002 and has since become one of the most widely prescribed antidepressants worldwide. It was developed as the active S-enantiomer of citalopram, allowing similar or better clinical benefits at lower doses, with improved tolerability and safety. Because of this, escitalopram is generally preferred over simply doubling the dose of citalopram. Its clinical importance is reflected in its inclusion on the World Health Organization’s List of Essential Medicines, a designation reserved for treatments considered effective, safe, and necessary for public health. By 2023, escitalopram had become the second most prescribed antidepressant and one of the most commonly prescribed medications overall in the United States, with tens of millions of prescriptions annually. Similar trends are seen globally, including Australia, where it has consistently ranked among the top prescribed medicines in recent years. In India, escitalopram is widely used in everyday psychiatric practice and is available under several familiar brand names such as Nexito, Cipralex, Escita, Zetalo, and others. While brand names may differ, the active medicine is the same, and treatment outcomes depend far more on correct dosing, consistency, and individual response than on the specific brand chosen.
Introduction
Starting a psychiatric medication can feel unsettling.
Many people who are prescribed escitalopram come to the clinic with mixed emotions—relief that there may finally be help, and fear about what the medicine might do to them. Questions often arise quietly, sometimes late at night:
Will this change who I am? Will I become dependent on it? Will I feel numb? What if I can’t stop it later?
These concerns are completely understandable. Much of the information available online is either overly reassuring or unnecessarily frightening, leaving very little room for nuance. The truth, as with most things in mental health, lies somewhere in between.
Escitalopram is one of the most commonly prescribed antidepressants worldwide. It has been studied extensively, used for decades, and prescribed to millions of people for conditions such as anxiety, depression, panic, and stress-related difficulties. Yet despite this, it is often poorly explained to patients.
This article is written to change that.
The aim here is not to convince you to take escitalopram, nor to dismiss your concerns. The aim is to help you understand the medication—what it does, what it does not do, what is common, what is rare, and how it is usually used thoughtfully in real clinical practice.
Mental health treatment works best when fear is replaced with clarity. When you know what to expect, your brain is less likely to interpret every sensation as danger. That alone can make treatment smoother and more effective.
If you have been prescribed escitalopram, are considering it, or are already taking it and have questions, this guide is meant to be a calm, reliable reference. It should support—not replace—discussion with your psychiatrist, because treatment decisions are always individual.
What does escitalopram do?
Escitalopram belongs to a group of medications called SSRIs (Selective Serotonin Reuptake Inhibitors).
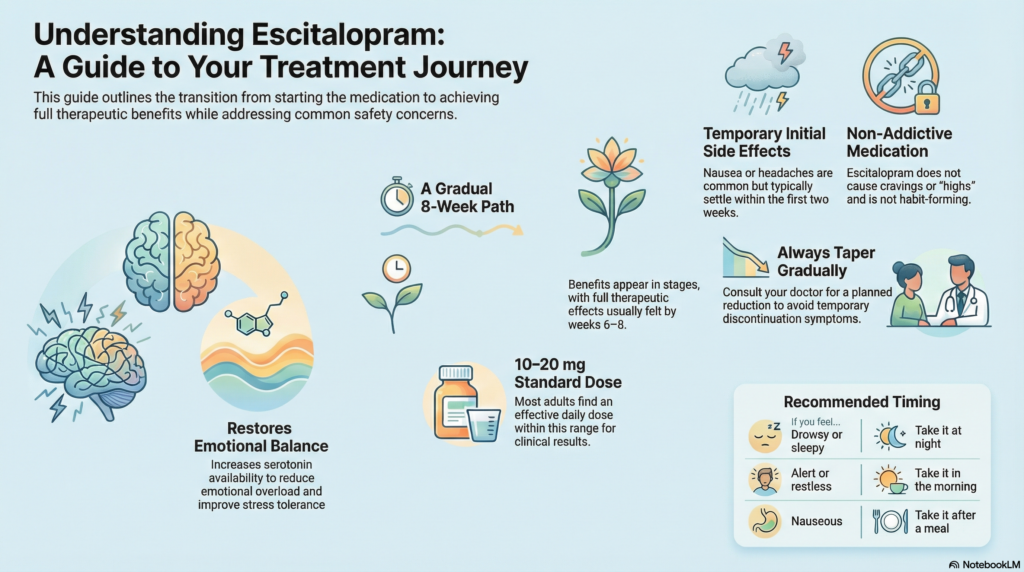
In simple terms, it:
-
Increases the availability of serotonin, a chemical involved in mood, anxiety regulation, emotional balance, and stress tolerance
-
Reduces excessive emotional reactivity
-
Helps the brain’s emotional circuits function more steadily
It does not artificially create happiness or suppress emotions.
Instead, it helps reduce emotional overload so that your natural personality can function better.
Escitalopram is commonly prescribed for:
-
Depression
-
Generalised anxiety disorder
-
Panic disorder
-
Social anxiety
-
Obsessive–compulsive symptoms
-
Stress-related emotional dysregulation
What is the usual dose range of escitalopram?
Doses are individualised based on symptoms, sensitivity, age, and response.
Typical ranges:
-
Starting dose: 5–10 mg once daily
-
Common effective dose: 10–20 mg once daily
-
Maximum dose (most adults): 20 mg per day
Many people respond well to lower doses, especially for anxiety. Increasing the dose is not always necessary and is done only if benefits clearly outweigh side effects.
Should escitalopram be taken with food or after food?
Escitalopram can be taken with food or without food.
However:
-
If you experience nausea or stomach discomfort, taking it after food is helpful
-
Food does not reduce its effectiveness
-
Take it at the same time each day for consistency
Does escitalopram make you drowsy or sleepy?
This varies from person to person.
-
Some people feel slightly sleepy or relaxed, especially in the first 1–2 weeks
-
Some feel mildly alert or activated
-
Most people feel neutral once the body adjusts
If it causes sleepiness:
-
Taking it at night usually helps
If it causes alertness or restlessness:
-
Taking it in the morning is better
This is a timing adjustment, not a dangerous reaction.
How long does escitalopram take to work?
Escitalopram works gradually, not immediately.
-
Week 1–2: Early side effects or mild anxiety reduction may appear
-
Week 2–4: Sleep, appetite, and emotional steadiness often improve
-
Week 4–6: Mood, motivation, and resilience improve
-
Week 6–8: Full therapeutic benefit is usually clear
Early lack of improvement does not mean the medication will not work.
Does escitalopram make you emotionally numb?
This is a very common concern.
Most people experience:
-
Reduced emotional overwhelm
-
Better regulation of emotions
-
Improved tolerance to stress
A small minority, usually at higher doses, may experience:
-
Emotional blunting
-
Feeling “flat” or less reactive
Important points:
-
This effect is dose-related
-
It is reversible
-
Dose adjustment or changing medication usually resolves it
Emotional numbness is not the goal of treatment.
What are the common side effects?
Most side effects are mild and temporary, especially in the first 1–2 weeks.
Common:
-
Nausea or gastric discomfort
-
Headache
-
Fatigue or mild restlessness
-
Sleep changes
-
Reduced libido or delayed ejaculation (in some people)
Less common:
-
Jaw tightness
-
Sweating
-
Brief increase in anxiety at the start
Most side effects settle as the brain adapts.
Does escitalopram cause dependence or addiction?
No.
Escitalopram does not:
-
Cause cravings
-
Produce a “high”
-
Lead to drug-seeking behaviour
-
Require increasing doses to feel normal
Needing to taper slowly does not mean addiction.
Will I have withdrawal symptoms if I stop escitalopram abruptly?
Stopping suddenly can cause discontinuation symptoms, especially after long-term use.
Possible symptoms include:
-
Dizziness
-
“Electric shock” sensations in the head
-
Irritability or anxiety
-
Sleep disturbance
-
Flu-like feelings
This happens because the brain is adjusting to a sudden change—not because of addiction.
To avoid this:
-
Escitalopram should be tapered gradually
-
Taper schedules depend on dose and duration
-
Most people stop comfortably with proper guidance
What is the risk of PSSD (Post-SSRI Sexual Dysfunction)?
PSSD refers to persistent sexual symptoms after stopping SSRIs. This topic can cause understandable anxiety online.
What is important to know:
-
PSSD appears to be rare
-
Most sexual side effects improve after dose reduction or stopping
-
The majority of patients fully recover
-
Risk may be higher with long-term high-dose use, but remains uncommon
Sexual function is influenced by many factors:
-
Anxiety and depression themselves
-
Stress
-
Sleep quality
-
Hormonal factors
-
Relationship issues
If sexual side effects occur, there are multiple management options, and early discussion helps reduce risk.
Are there alternatives to escitalopram?
Yes. Escitalopram is one option among many.
Alternatives may include:
-
Other SSRIs
-
SNRIs
-
Atypical antidepressants
-
Psychological therapies
-
Sleep-focused interventions
-
Neurofeedback
-
Combined approaches
The best choice depends on the individual—not the diagnosis alone.
Is escitalopram safe during pregnancy or breastfeeding?
This requires an individualised risk–benefit discussion.
-
Escitalopram is commonly used when clinically necessary
-
Untreated depression or anxiety also carries risks
-
Decisions depend on symptom severity, history, and alternatives
Never stop medication suddenly during pregnancy without medical guidance.
How long will I need to take escitalopram?
This varies:
-
First episode: usually 6–12 months after recovery
-
Recurrent episodes: sometimes longer
-
Anxiety disorders: duration depends on relapse risk
Stopping medication is a planned, gradual process.
Final thoughts
Escitalopram is neither something to fear nor something to take casually.
When prescribed thoughtfully, monitored properly, and reviewed regularly, it is a safe and effective tool for many people.
Good psychiatric care focuses on:
-
The right diagnosis
-
The right dose
-
The right duration
-
The right combination of treatments
Clear understanding reduces fear—and fear reduction itself is therapeutic.
About the author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic – Apollo Clinic Velachery (Opp. Phoenix Mall)
I provide evidence-based psychiatric care integrating medication, psychotherapy, sleep science, and modern neuropsychiatry—tailored to each individual.
✉ srinivasaiims@gmail.com
📞 +91-8595155808