IBS: Diagnosis and Treatment Guidelines
 🩺 Understanding IBS: More Than Just a Gut Issue
🩺 Understanding IBS: More Than Just a Gut Issue
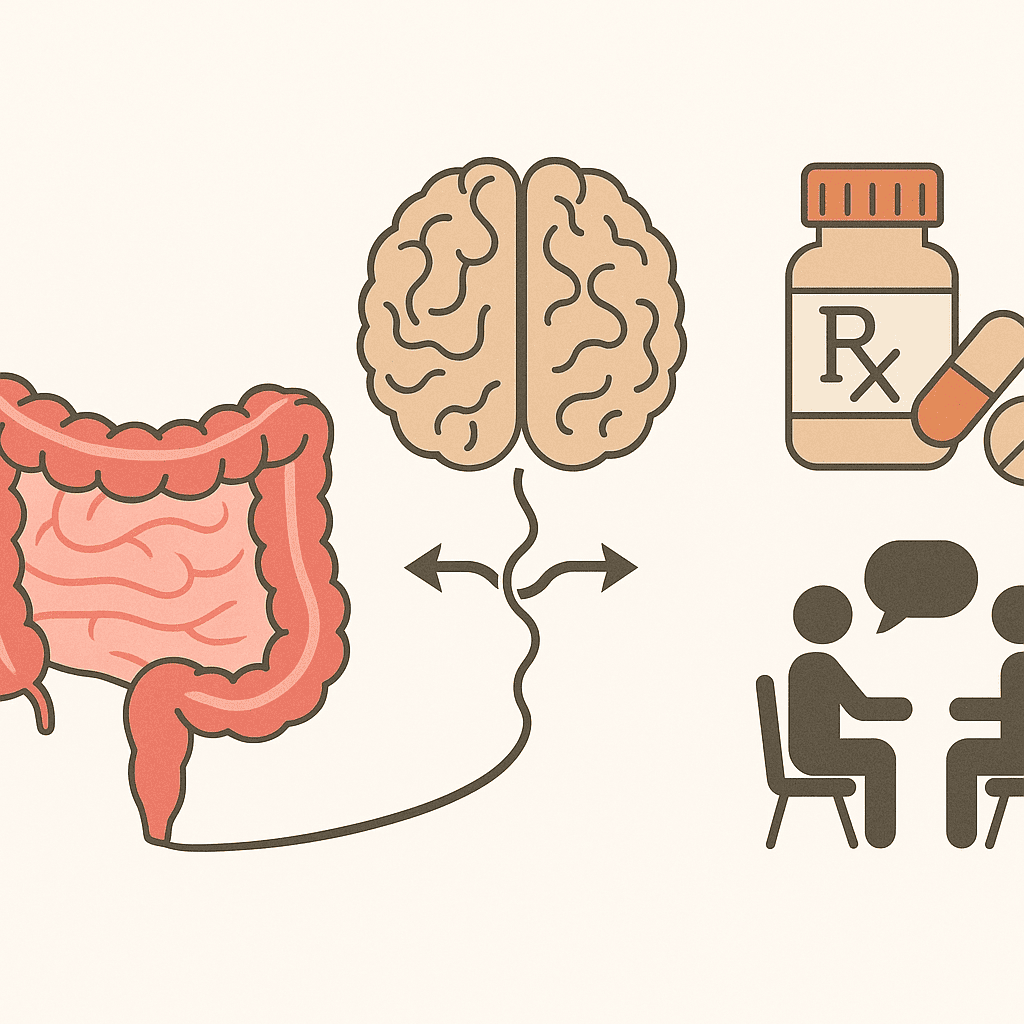
Irritable Bowel Syndrome (IBS) is one of the most common yet misunderstood conditions seen in both gastroenterology and psychiatry clinics. Characterized by abdominal discomfort and altered bowel habits, IBS is a functional gastrointestinal disorder—meaning its symptoms arise from abnormal communication between the gut and the brain rather than from structural disease. Despite lacking visible abnormalities on scans or endoscopy, the condition can significantly impair quality of life. Modern guidelines emphasize a multifaceted approach—diagnosing IBS accurately, classifying its subtypes, ruling out red flags, and offering tailored treatment that addresses both physical and psychological dimensions.
🧩 Diagnosis of IBS
➤ Rome IV Diagnostic Criteria:
-
Recurrent abdominal pain (≥1 day/week for the last 3 months), associated with at least 2 of the following:
-
Related to defecation
-
Change in stool frequency
-
Change in stool form (appearance)
-
Symptoms must have started ≥6 months before diagnosis.
➤ Alarm (Red Flag) Symptoms:
-
Age >50 with new symptoms
-
GI bleeding or anemia
-
Nocturnal diarrhea
-
Weight loss
-
Family history of colorectal cancer, IBD, or celiac disease
➤ Initial Investigations:
-
CBC, CRP, Celiac serology
-
Fecal calprotectin (if IBD suspected)
-
Colonoscopy if red flags or age >45–50
🔄 IBS Subtypes (Based on Bristol Stool Scale)
| Subtype | Stool Pattern |
|---|---|
| IBS-D | Diarrhea predominant |
| IBS-C | Constipation predominant |
| IBS-M | Mixed pattern |
| IBS-U | Unsubtyped |
💊 Treatment Guidelines
🟩 General Measures:
-
Patient education and reassurance
-
Low FODMAP diet (under dietician supervision)
-
Regular meals, hydration, exercise
-
Stress and mental health evaluation
🟧 IBS-C:
-
Soluble fiber (psyllium)
-
PEG, lactulose
-
Secretagogues: linaclotide, lubiprostone
-
SSRIs for coexisting anxiety/depression
🟦 IBS-D:
-
Loperamide
-
Bile acid sequestrants (cholestyramine)
-
Rifaximin (14-day course)
-
Eluxadoline (if no biliary disease)
-
Low-dose TCAs (e.g., amitriptyline 10–25 mg)
🟨 IBS-M:
-
Symptom-specific strategy
-
Consider TCA or SSRI
-
Integrate psychological support
🧠 Psychiatric & Behavioral Management
| Strategy | Role |
|---|---|
| CBT | First-line for gut-focused anxiety, catastrophizing, and symptom preoccupation |
| Mindfulness & Hypnotherapy | Effective in reducing gut sensitivity |
| Psychotropic Medications | TCAs (IBS-D), SSRIs/SNRIs (IBS-C/pain), benzodiazepines (short-term only) |
| Screening Tools | PHQ-9, GAD-7, IBS-SSS |
🤝 Multidisciplinary Care
-
Gastroenterologist: Workup and initial diagnosis
-
Psychiatrist: Treat comorbid anxiety, depression, somatization
-
Psychologist: Deliver structured therapies like CBT
-
Dietician: Implement Low FODMAP or fiber adjustment plans
🚫 Not Routinely Recommended
-
Long-term antibiotics (except rifaximin)
-
Routine probiotics (unless strain-specific)
-
Long-term benzodiazepines
-
Empirical colonoscopy without red flags
✅ Summary Table
| Component | Recommendation |
|---|---|
| Diagnosis | Rome IV + symptom screen + minimal labs |
| Diet | Low FODMAP (under supervision) |
| Medication | Tailored to IBS subtype |
| Mental Health | Screening + CBT + psychotropics where needed |
| Referral | Alarm symptoms, refractory cases |
📣 Need Help Managing IBS Holistically?
If you’re struggling with ongoing digestive issues, stress, or mood symptoms that seem to fuel your IBS flares—help is available.
I specialize in the mind-gut connection, offering integrated psychiatric care for IBS, anxiety, and related disorders. Treatment plans are personalized, collaborative, and evidence-based.
Dr. Srinivas Rajkumar T
MD (AIIMS, New Delhi), Consultant Psychiatrist
📍 Apollo Clinic, Opp. Phoenix Marketcity, Velachery, Chennai
☎️ +91 8595155808
🌐 www.srinivasaiims.com
Related posts:
- IBS and Mental Health: Understanding the Gut–Mind Axis and Modern Psychiatric Treatment
- Adult ADHD: Assessment, Diagnosis, Differential Diagnosis, and Treatment
- Vishaka Guidelines – Sexual Harassment at Workplace – India
- Media Guidelines on Suicide Reporting – India
- Telemedicine Practice Guidelines 2020: A Simplified Guide for Psychiatrists
- Navigating the Future of Healthcare: Understanding ICMR’s Ethical Guidelines for AI in Healthcare Research