Managing Treatment-Resistant Depression (TRD)
 If you or someone close to you is living with depression and finding that standard antidepressants aren’t bringing the relief you hoped for, you are not alone—and you are not failing treatment.
If you or someone close to you is living with depression and finding that standard antidepressants aren’t bringing the relief you hoped for, you are not alone—and you are not failing treatment.
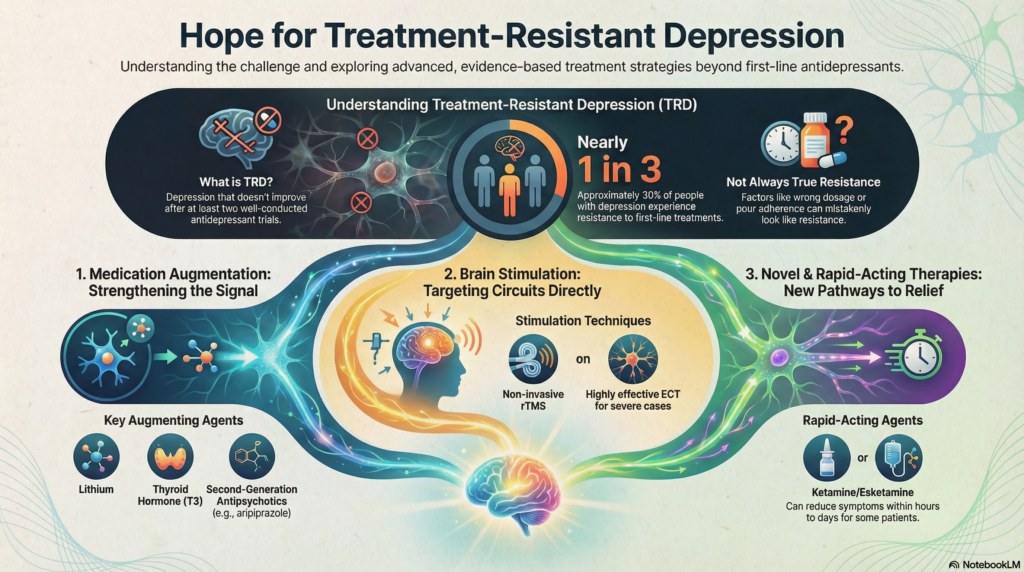
Major Depressive Disorder (MDD) is not a single illness with a single cause. It is a heterogeneous condition, shaped by biology, psychology, life stressors, and brain circuitry. While many people respond well to first-line treatments, nearly one in three individuals (≈30%) continue to experience significant symptoms despite appropriate care.
When this happens, clinicians refer to the condition as Treatment-Resistant Depression (TRD).
The good news is this: TRD does not mean untreatable. It simply means the approach needs to become more systematic, layered, and precise.
What Is Treatment-Resistant Depression?
In psychiatry, Treatment-Resistant Depression is commonly defined as an inadequate response to at least two well-conducted trials of antidepressants, given at adequate doses and duration.
Several staging systems attempt to quantify the degree of resistance—such as the Maudsley Staging Method (MSM) or the Thase and Rush model—but clinically, the emphasis is less on labels and more on understanding why treatment hasn’t worked yet.
Importantly, not all apparent resistance is true resistance. A significant proportion of cases fall into what we call pseudo-resistance, where improvement was unlikely from the outset due to remediable factors such as:
-
Suboptimal dosing – the medication was never pushed to a therapeutic range
-
Premature discontinuation – stopping before the 6–8 week window needed for response
-
Poor adherence – inconsistent intake, often due to side effects or unclear expectations
-
Unrecognised comorbidities – anxiety disorders, substance use, personality vulnerabilities, sleep disorders, or medical conditions that blunt antidepressant response
Clarifying these factors is not “going backward”—it is often the fastest way forward.
Evidence-Based Strategies for Treatment-Resistant Depression
When first-line treatments are insufficient, psychiatry offers several well-validated next steps, each targeting different biological and neural pathways.
1. Medication Augmentation: Strengthening the Signal
Rather than switching endlessly between antidepressants, augmentation involves adding a second agent that enhances the antidepressant effect through a different mechanism.
-
Lithium
One of the most robustly supported augmentation strategies. Lithium is as effective as many second-generation antipsychotics and has a unique anti-suicidal effect, making it especially valuable in high-risk patients. -
Thyroid Hormone (T3)
Triiodothyronine can accelerate and amplify antidepressant response, even in patients with normal thyroid function. It is generally well tolerated and requires less intensive monitoring than lithium. -
Second-Generation Antipsychotics (SGAs)
Agents such as quetiapine, aripiprazole, and olanzapine have strong evidence in TRD when used judiciously. Their benefit lies not only in dopamine modulation but also in effects on serotonin, glutamate, and emotional regulation circuits.
2. Brain Stimulation Therapies: Targeting Circuits Directly
Depression is increasingly understood as a disorder of neural networks, particularly involving the prefrontal cortex, limbic system, and their connectivity. Brain stimulation therapies aim to recalibrate these circuits.
-
Repetitive Transcranial Magnetic Stimulation (rTMS)
A non-invasive technique that uses magnetic pulses to modulate cortical activity. In TRD, rTMS is several times more effective than sham treatment, with sustained benefits in many patients. -
Theta-Burst Stimulation (TBS)
A newer, time-efficient form of rTMS that mimics natural brain rhythms. An intermittent TBS (iTBS) session lasts about 3 minutes and has comparable efficacy to traditional protocols. -
Electroconvulsive Therapy (ECT)
Despite persistent stigma, modern ECT remains the most effective treatment for severe and resistant depression, with response rates approaching 70–75%, especially in melancholic, psychotic, or life-threatening depression. -
Magnetic Seizure Therapy (MST)
An emerging technique that induces a seizure using magnetic fields rather than electricity. Early data suggest ECT-level efficacy with fewer cognitive side effects, though availability remains limited.
3. Rapid-Acting and Novel Therapies
Traditional antidepressants work slowly by altering monoamine signaling. Newer treatments act on glutamate, inflammation, and inhibitory neurotransmission, offering faster relief for select patients.
-
Ketamine and Esketamine
These agents can produce meaningful symptom reduction—and reduction in suicidal ideation—within hours to days. Intranasal esketamine is now approved for restricted use in TRD under supervised settings. -
Anti-Inflammatory Approaches
A subset of patients with elevated inflammatory markers (such as CRP) show preferential response to targeted anti-inflammatory strategies, highlighting the role of immune-brain interactions in depression. -
GABA-Modulating Agents
New compounds acting on the brain’s primary inhibitory system have demonstrated high response rates in recent trials, particularly in patients with anxiety-laden or stress-sensitive depression.
Moving Forward: From Trial-and-Error to Strategy
Treatment-Resistant Depression is not a dead end—it is a signal to shift from linear prescribing to strategic formulation.
Using structured tools like the Antidepressant Treatment History Form (ATHF) allows clinicians to map what has been tried, what has truly failed, and what remains unexplored. This reduces unnecessary repetition and guides a more rational, personalized treatment plan.
Recovery from TRD often happens not through a single dramatic intervention, but through sequencing the right treatments, in the right order, for the right patient.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi)
Consultant Psychiatrist
Dr. Srinivas Rajkumar T is a Chennai-based psychiatrist with a special interest in treatment-resistant mood disorders, complex psychopharmacology, and modern brain-based interventions. His clinical approach integrates biological, psychological, and neurocircuit-level understanding to help patients who have not responded to conventional treatments.
Apollo Clinic Velachery (Opp. Phoenix Mall)
📧 srinivasaiims@gmail.com
📞 +91-8595155808