QEEG-Led Clinical Breakthrough: Primary vs Secondary Negative Symptoms in Schizophrenia
 Negative symptoms are the quiet crisis of schizophrenia.
Negative symptoms are the quiet crisis of schizophrenia.
They don’t shout like hallucinations.
They don’t alarm like catatonia.
But they decide whether a person returns to life or remains frozen outside it.
And yet, one of the most damaging mistakes in clinical psychiatry is this:
Assuming all negative symptoms are the same.
They are not.
This is the story of how QEEG changed a clinical dead-end into a treatment breakthrough by helping distinguish primary from secondary negative symptoms in schizophrenia.
The Clinical Problem We All Face
A patient with schizophrenia stabilises:
-
No hallucinations
-
No delusions
-
No agitation
But instead, we see:
-
Flat affect
-
Reduced speech
-
Poor motivation
-
Social withdrawal
-
Cognitive slowing
The reflex diagnosis?
“Residual negative symptoms.”
“Deficit schizophrenia.”
“Poor prognosis.”
And the reflex response?
-
Increase antipsychotic dose
-
Add another drug
-
Accept stagnation
This is where many recoveries quietly die.
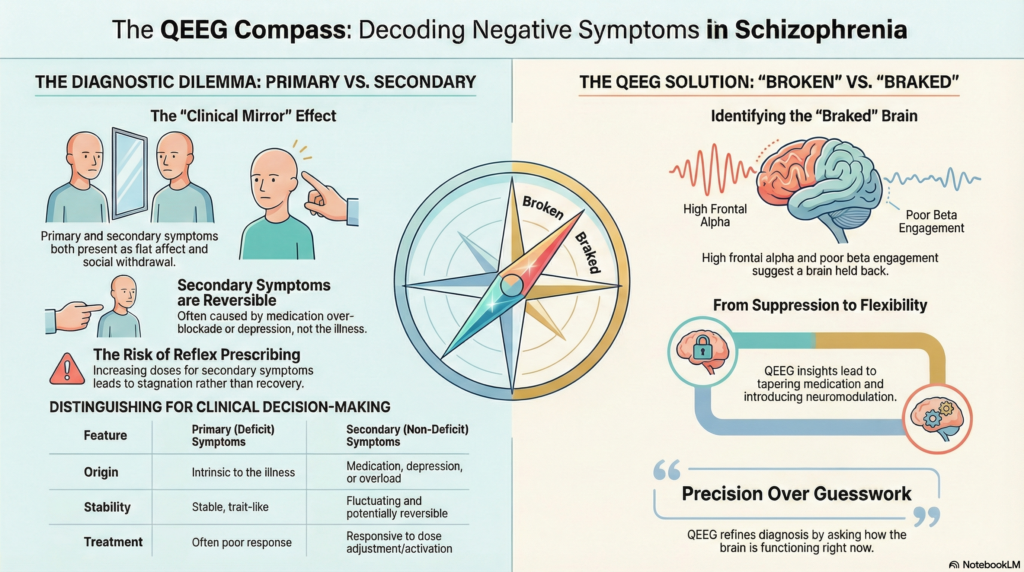
Primary vs Secondary Negative Symptoms — The Forgotten Divide
Modern psychiatry clearly distinguishes two entities:
Primary (Deficit) Negative Symptoms
-
Intrinsic to the illness
-
Present early, often premorbid
-
Stable, trait-like
-
Poor response to treatment
Secondary Negative Symptoms
-
Caused by:
-
Medication over-blockade
-
Post-psychotic recovery state
-
Depression or anxiety
-
Cognitive overload
-
-
Potentially reversible
Clinically, they look identical.
Neurobiologically, they are very different.
The challenge has always been:
How do we tell them apart in real patients?
Where QEEG Changed the Game
In a young man with:
-
Acute onset psychosis (ATPD-like)
-
Catatonia with food refusal
-
Short duration of illness (≈1.5 years)
-
Complete remission of positive symptoms
-
Severe PANSS negative score (N = 40)
The question was critical:
Is this deficit schizophrenia
or secondary negative suppression?
Enter Quantitative EEG (QEEG)
Instead of asking what symptoms look like, QEEG asks:
How is the brain functioning right now?
What the QEEG Revealed
Not degeneration.
Not disorganisation.
Not cortical damage.
Instead:
-
Preserved dominant alpha rhythm (~10 Hz)
-
Excess frontal alpha during eyes-open state
-
Poor task-related beta engagement
-
Inadequate theta–beta modulation
-
Failure of cortical “state switching”
In plain terms:
The brain was intact — but under-mobilised.
This is the signature of secondary negative symptoms.
A brain that can engage, but is being held back.
Why This Matters Clinically
If this were primary deficit schizophrenia, QEEG would often show:
-
Generalised slowing
-
Poor rhythmic integrity
-
Reduced reactivity across states
That was not the case.
Instead, the QEEG told us:
“This brain does not need more suppression.
It needs flexibility.”
That single insight changed everything.
The Treatment Breakthrough
Instead of escalating medication:
-
We reframed the diagnosis
-
Recognised dopaminergic over-suppression
-
Identified secondary negative symptoms
What changed in management
-
Cross-tapered high-dose risperidone
-
Introduced a lower-EPS antipsychotic
-
Planned neuromodulation (tDCS, neurofeedback)
-
Shifted focus to cognitive activation and recovery
This was not guesswork.
It was QEEG-guided clinical reasoning.
Why This Is Bigger Than One Case
This is not about EEG gadgets.
It’s about precision psychiatry.
QEEG helps answer questions we’ve struggled with for decades:
-
Is the brain broken or braked?
-
Should we add medication — or remove it?
-
Is stagnation illness-driven or treatment-induced?
Used correctly, QEEG does not replace diagnosis.
It refines it.
A Word of Caution
QEEG is not magic.
-
It does not diagnose schizophrenia
-
It does not replace clinical judgment
-
It must be interpreted in context
But when combined with:
-
Longitudinal history
-
PANSS profiling
-
Cognitive testing
-
Medication review
It becomes a powerful clinical compass.
The Take-Home Message
Not all negative symptoms mean decline.
Not all flatness means deficit.
Not all silence means loss.
Sometimes, it means:
The brain is waiting to be released.
QEEG helps us see that difference — and act on it.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
I work at the intersection of clinical psychiatry, neurophysiology, and recovery-oriented care, using tools like QEEG, neurofeedback, and neuromodulation to move beyond symptom control toward functional restoration.
📍 Chennai
📞 +91-8595155808
✉ srinivasaiims@gmail.com
🌐 srinivasaiims.com