Sleep Series: Men, Women, and Sleep: Why One-Size-Fits-All Advice Fails
 Sleep advice is usually delivered in neutral language.
Sleep advice is usually delivered in neutral language.
“Adults need 7–8 hours.”
“Maintain a regular sleep schedule.”
“Avoid screens at night.”
It sounds universal. Scientific. Fair.
And yet, when you look closely at how sleep problems actually present in clinics—and how sleep patterns relate to long-term health—the idea of gender-neutral sleep advice begins to fall apart.
Men and women do not sleep the same way, do not lose sleep for the same reasons, and do not carry the same risks when sleep goes wrong.
Different Bodies, Different Sleep Biology
At a biological level, sleep regulation is influenced by:
-
Hormonal rhythms
-
Stress responsivity
-
Circadian timing
-
Social roles and expectations
These influences differ meaningfully between men and women across the lifespan.
Women, for example, experience repeated hormonal transitions—menstrual cycles, pregnancy, postpartum changes, perimenopause, menopause—each of which alters sleep architecture and circadian stability. Men, in contrast, tend to show earlier circadian timing and higher rates of sleep-disordered breathing.
These differences matter. They shape not only how sleep problems arise, but how they affect health over time.
What the Evidence Is Quietly Showing
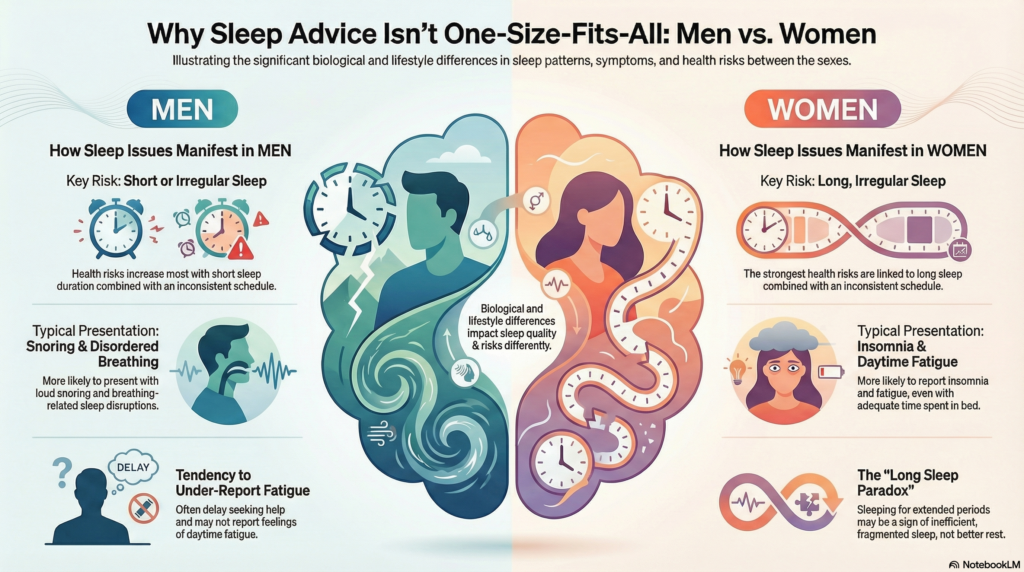
Recent large population studies examining sleep duration and regularity have revealed striking sex-specific patterns.
In men, health risk increases notably with:
-
Short sleep combined with irregular timing
-
Long sleep, even when sleep timing appears regular
In women, the strongest risk emerges with:
-
Long sleep combined with irregular timing
-
Sleep patterns marked by fatigue rather than overt sleepiness
The implication is subtle but powerful: the same sleep pattern does not carry the same meaning—or risk—in men and women.
How Sleep Problems Present Differently
Men are more likely to present with:
-
Loud snoring or breathing-related sleep disruption
-
Short sleep due to work schedules
-
Under-reporting of fatigue
-
Delayed help-seeking
Women are more likely to present with:
-
Insomnia despite adequate time in bed
-
Daytime fatigue rather than sleepiness
-
Sleep disruption linked to stress, caregiving, or hormonal change
-
Greater sensitivity to irregular sleep timing
As a result, women are often told they are “sleeping enough” because their hours look adequate—while their sleep quality continues to deteriorate.
The Long Sleep Paradox in Women
One of the more intriguing and concerning patterns is the association between long, irregular sleep and health risk in women.
This does not suggest that women should sleep less. It suggests that:
-
Prolonged sleep may reflect fragmented or inefficient sleep
-
Irregular timing amplifies circadian disruption
-
Fatigue drives compensatory behaviours that worsen sleep regulation
In clinical terms, this is often the woman who sleeps nine hours, wakes exhausted, pushes through the day, and collapses into bed early—perpetuating the cycle.
Without addressing rhythm and efficiency, the problem quietly deepens.
Why Standard Advice Often Misses the Mark
Generic sleep advice tends to:
-
Focus on duration over timing
-
Ignore hormonal and caregiving realities
-
Underestimate the impact of irregularity
-
Treat fatigue as a minor symptom rather than a signal
This is why well-intentioned advice can fail—or even backfire—particularly for women.
Sleep needs context. Biology does not operate in averages.
Clinical Implications: Treating Sleep, Not Stereotypes
Effective sleep intervention requires:
-
Asking different questions of men and women
-
Paying attention to fatigue, not just sleepiness
-
Evaluating long sleep as a potential warning sign
-
Prioritising circadian stability over time-in-bed extension
Approaches like CBT-I work precisely because they adapt to these realities. They target timing, arousal, and efficiency rather than chasing a fixed number of hours.
Sleep improves not when advice is equal—but when it is appropriate.
The Takeaway
Sleep is biological, but it is not generic.
Men and women live in different physiological and social rhythms, and their sleep reflects that truth. Ignoring these differences does not create fairness—it creates blind spots.
Understanding sleep through a sex-informed lens allows us to intervene earlier, treat more precisely, and prevent long-term harm.
In the next article, we’ll explore how sleep changes across the lifespan—and why advice that works at 30 can fail spectacularly at 60.
Reference
Park SJ, Park J, Kim BS, Park J-K. The impact of sleep health on cardiovascular and all-cause mortality in the general population. Scientific Reports. 2025;15:30034.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA
Consultant Psychiatrist & Neurofeedback Specialist
Dr. Srinivas specialises in sleep-related psychiatric care, with a focus on insomnia, circadian rhythm disorders, and sleep disturbances linked to mood, anxiety, and neurodevelopmental conditions. His work integrates CBT-I, rhythm stabilisation, and neurobiological insight to achieve durable sleep improvement.
📍 Apollo Clinic Velachery (Opp. Phoenix Mall), Chennai
✉ srinivasaiims@gmail.com
📞 +91-8595155808