The Rise of Neurostimulation in ADHD Treatment
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental condition affecting both children and adults. Traditional treatments like stimulants and non-stimulants have long been the cornerstone of ADHD management. However, concerns over medication side effects, adherence challenges, and limited long-term efficacy have fueled interest in non-pharmacological interventions. Among these, neurostimulation is emerging as a promising alternative. A recent systematic review and network meta-analysis published in The Lancet Psychiatry sheds light on the comparative efficacy and acceptability of neurostimulatory interventions for ADHD in adults (Ostinelli et al., 2025).
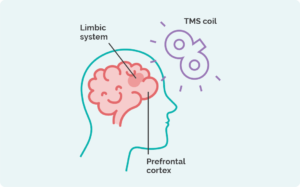
What Is Neurostimulation?
Neurostimulation involves non-invasive techniques like transcranial direct current stimulation (tDCS) and transcranial magnetic stimulation (TMS). These methods modulate brain activity by targeting specific neural circuits responsible for attention, executive function, and impulse control—key areas affected in ADHD.
Key Findings from the Meta-Analysis
1. Efficacy of Neurostimulation
Neurostimulation, particularly tDCS, showed significant benefits in reducing core ADHD symptoms when measured by clinician-reported scales. The study found that:
- tDCS was more effective than placebo at 12 weeks, with a standardized mean difference (SMD) of -0.78 (95% CI: -1.13 to -0.43).
- Other non-pharmacological interventions, such as cognitive behavioral therapy (CBT) and mindfulness, also demonstrated effectiveness, but neurostimulation offers a more direct neural approach (Ostinelli et al., 2025).
2. Safety and Acceptability
While stimulants like methylphenidate and atomoxetine remain highly effective, they were associated with higher discontinuation rates due to adverse effects. In contrast, neurostimulation displayed excellent tolerability, making it an attractive option for individuals seeking medication-free treatments.
3. Discrepancy in Perceived Benefits
Interestingly, self-reported measures did not always align with clinician-reported improvements. This suggests that while patients may not immediately perceive changes, neurostimulation produces measurable neural and behavioral benefits.
Why Neurostimulation Matters
- Non-Invasive and Drug-Free: Neurostimulation provides a medication-free option, reducing risks of dependency and side effects.
- Targeted Therapy: By focusing on specific brain regions, neurostimulation addresses the underlying neurobiology of ADHD.
- Complementary Approach: It can be used alongside traditional therapies, enhancing overall treatment outcomes.
Real-World Applications
Transcranial Direct Current Stimulation (tDCS):
- Affordable and portable, making it suitable for home-based treatments.
- Requires minimal supervision, offering convenience for patients.
Transcranial Magnetic Stimulation (TMS):
- Effective in stimulating deeper brain regions.
- Typically administered in clinical settings, ideal for treatment-resistant cases.
Challenges and Future Directions
- Long-Term Efficacy: Most studies, including Ostinelli et al. (2025), focus on short-term outcomes. Long-term research is crucial to determine sustained benefits.
- Individual Variability: Responses to neurostimulation vary, highlighting the need for personalized protocols.
- Integration with Traditional Therapies: Combining neurostimulation with behavioral therapies like CBT could maximize benefits.
Conclusion
Neurostimulation is revolutionizing ADHD treatment by offering a non-invasive, effective, and well-tolerated option. While traditional medications remain essential, incorporating neurostimulatory interventions like tDCS and TMS can diversify and enhance treatment plans, especially for adults seeking alternatives to medication. As research progresses, neurostimulation holds promise as a cornerstone of personalized ADHD care.
References
Ostinelli EG, Schulze M, Zangani C, Farhat LC, Tomlinson A, Del Giovane C, et al. Comparative efficacy and acceptability of pharmacological, psychological, and neurostimulatory interventions for ADHD in adults: a systematic review and component network meta-analysis. Lancet Psychiatry. 2025;12:32–43.